What is shoulder osteoarthritis (OA)?
Osteoarthritis (OA) of the shoulder (known as the gleno-humeral joint) causes pain and restriction in movement of the shoulder. It is often worse in the mornings and improves with gentle activity and exercise. It can cause you to wake up at night with pain. Pain is aggravated by moving your arm out to the side and above your head. Shoulder osteoarthritis predominantly effects those over 50 years of age, women more commonly than men and those with a familial history. It is diagnosed using a series of clinical tests and imaging. Osteoarthritis is best managed with physiotherapy, however if the pain is too severe to carry out exercise based treatment and/or is waking you at night then an ultrasound guided steroid injection is a very effective treatment option for rapid pain relief.
What are the symptoms of osteoarthritis of the shoulder?
The symptoms of osteoarthritis of the shoulder are:
- Pain and stiffness of the shoulder- often quite diffuse, achy pain deep in the joint
- Intermittent sharp pan with overhead movements and associated grinding and audible cracking/clicking in the joint
- Pain is worse in the morning and eases with gentle movement
If this sounds like your pain, read on…
What other conditions can mimic osteoarthritis of the shoulder?
If this does not sound like your pain there are other conditions that can mimic the pain of osteoarthritis of the shoulder such as:
- acromio-clavicular (AC) joint osteoarthritis
- frozen shoulder
- shoulder impingement
- rotator cuff pain
- sub-acromial bursitis
Shoulder joint osteoarthritis (OA) versus frozen shoulder?
Osteoarthritis of the shoulder joint is more common in those over 50 or 60 years old, whereas frozen shoulder effects those between 40-60 years old. Frozen shoulder is very rare over the age of 60, unless it has developed after surgery or a fall. Both conditions present with a similar restriction in movement and are often worse at night and in the mornings. An X-ray is essentially normal with a frozen shoulder, whereas osteoarthritis is clearly demonstrated on an X-ray.
Anatomy
The shoulder connects the upper limb to the body and consists of four joints, two of which are commonly affected by osteoarthritis. The two joints in question are:
- The glenohumeral joint. This joint is created by the ball-shaped end of the humerus (long bone or the upper arm) and a shallow dish (called the glenoid) which is located on the shoulder blade (scapula). This articulation forms a ball and socket joint and is responsible for producing the wide variety of movements possible at the shoulder.
- The acromioclavicular joint. This small joint is located towards the tip of your shoulder and attaches the clavicle (collarbone) to the acromion (front aspect of the shoulder blade). This joint produces small, simple sliding movements required to adjust the shoulder blade position during movement.
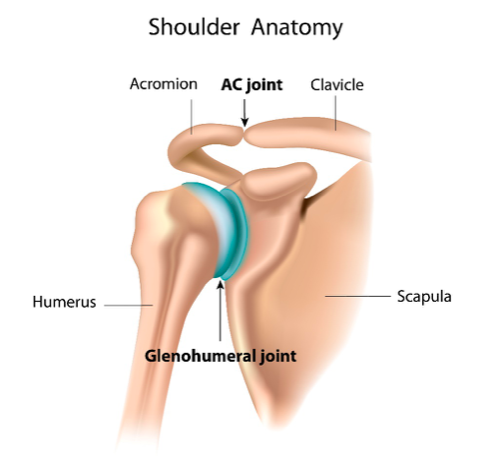
The glenohumeral and acromioclavicular joints work together to stabilise the shoulder whilst at the same time synergistically moving to create the series of complex and fluid arm movements. This is critical to nearly all our activities of daily living.
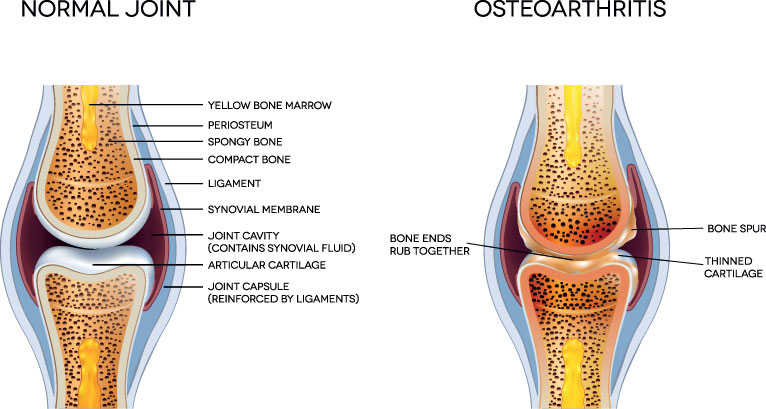
Both the glenohumeral and acromioclavicular joint surfaces are protected by a layer of articular cartilage.
Articular cartilage provides the joint with a friction free surface during arm movement and protects the underlying bone ends from damage. If either joint is subjected to adverse stress this protective layer become thinner and over time the thin layer of articular cartilage can become disrupted. This progressive, degenerative joint alteration is called osteoarthritis.
Repetitive movements of an osteoarthritic shoulder joint can cause inflammation of the surrounding soft tissue and joint lubricant (synovium). This inflammatory process is called synovitis.
What are the causes of shoulder osteoarthritis?
The exact cause is unknown. It is far less common than knee and hip osteoarthritis. There are certain risk factors that can predispose you to osteoarthritis. These can be:
- Age – more often occurs in those > 50
- Sex – more common in females
- Family history – osteoarthritis can run in the family
- Weight – a higher than normal body mass index (BMI) is associated with osteoarthritis in the shoulder
- Previous trauma e.g. a previous fracture or dislocation of the shoulder. This is known as post-traumatic osteoarthritis
- Certain occupations e.g. those involving heavy lifting such as construction work
- Smoking – is linked to poor joint health
How do you know if you have shoulder osteoarthritis?
Symptoms of osteoarthritis start with an intermittent deep ache within the shoulder, often during overhead activities. As osteoarthritis develops, symptoms can become increasingly painful and more frequent. Symptoms normally can become constant, affecting activities of daily living also causing you to wake at night.
Common symptoms of shoulder osteoarthritis include:
- Dull aching pain located deep within the shoulder.
- Occasional episodes of sharp pain. These are commonly associated with synovitis within the joint.
- Sensation of grinding or an audible clicking sound within the shoulder joint during movements.
- Reduced range of movement and joint stiffness first thing in the morning. This resolves quickly with movement. As osteoarthritis progresses shoulder movement can become more pronounced, limiting overhead activities.
How is osteoarthritis of the shoulder diagnosed?

If you feel may have osteoarthritis in your shoulder it is recommended that you seek professional advice.
A diagnosis of shoulder joint osteoarthritis is initially made by analysing the history of your symptoms and completing a combination of strength and range of movement tests. This can be undertaken by either a physiotherapist or an orthopaedic consultant.
If after completing a clinical assessment your clinician believes you may have osteoarthritis in your shoulder, you may be referred for x-ray. X-ray imaging has been used extensively for many decades to assess bone and joint pathology and is excellent at assessing the presence and the severity of osteoarthritis. You may also be asked to have a series of blood tests. Blood tests are used to rule out other pathologies such as systemic inflammation associated with rheumatoid arthritis.
Although x-ray is an excellent modality for diagnosing osteoarthritis, it is not capable of assessing the soft tissue inflammation associated with synovitis. Many patients suffering from osteoarthritis of the shoulder have symptoms which do not correlate with the severity of the disease seen on x-ray. This is often due to the presence of synovitis within the shoulder joint which is not observed on x-ray imaging.
Research has shown diagnostic musculoskeletal ultrasound imaging is an excellent diagnostic tool to accurately assess bony changes associated with osteoarthritis. It is also capable of assessing the presence of the swelling and inflammation associated with synovitis (Kaeley el at, 2020). Synovitis is often responsible for the acute spike of pain frequently experienced in an osteoarthritic joint and is believed to be associated with disease progression.
Complete has a team of highly experienced physiotherapists who are skilled in the assessment and diagnosis of osteoarthritis of the shoulder. All our clinicians are also fully qualified musculoskeletal sonographers. During the initial assessment you will be taken through a complex series of clinical tests and undergo a diagnostic musculoskeletal ultrasound scan.
If you would like more information or would like to book an appointment please contact us on 0207 4823875 or email injections@complete-physio.co.uk.
How do we treat osteoarthritis of the shoulder?
Most patients respond very well to conservative management for the treatment of osteoarthritis of the shoulder. Conservative management often consists of over-the-counter pain medication and a course of physiotherapy. Current research states that flexibility and strength are the most important factors in the management of osteoarthritis (Gross et al, 2019) and therefore, treatment programs are designed to:
- Increase range of movement. This is achieved using a combination of stretches and occasionally manual therapy techniques to manipulate your shoulder joint.
- Increasing strength in the surrounding shoulder muscles.

Here are some exercises you may like to try:
- Modify or avoid activities which aggravate your pain. This may involve taking regular breaks or splitting tasks up into smaller manageable tasks.
- Start a stretching program for your shoulder joint. Walking your fingers up a wall is a good way to start stretching the shoulder joint. Hold your stretch 30 seconds before repeating.
- Try some gentle arm strengthening exercises.
Over-the-counter medication such as paracetamol or a nonsteroidal anti-inflammatory gel such as Voltarol can be effective methods of reducing pain in arthritic joints. Discuss the use of medication with your pharmacist before starting treatment.
What if conservative management does not work?
Occasionally, conservative management is not successful in resolving symptoms. If this is the case, there are other treatment options available to you. These will be discussed below.
Injection therapy
If your pain remains significant and is affecting the following activities injection therapy may be beneficial for you.
- Pain that is affecting your ability to sleep or waking you at night.
- Pain that is stopping you from completing normal tasks such as washing and dressing or leisure activities.
- Pain that is limiting your ability to undertake in physiotherapy rehabilitation.
Injection therapy for the management of osteoarthritis of the shoulder is routinely used and has been proven to be an effective treatment for reducing the pain associated with joint pathology. An injection is performed to reduce pain and inflammation and allow a ‘window of opportunity’ for you to rehabilitate your shoulder effectively. It is recommended, that for best results, a course of physiotherapy is commenced within two weeks of receiving a shoulder injection.
Current research has revealed that injections completed under ultrasound guidance are more accurate at delivering the medication to the target tissue and more effective at reducing pain and increasing function than landmark guided injections (Daniels et al, 2018).
At Complete all our clinicians are fully qualified at performing ultrasound-guided injections and a highly experienced in the treatment of osteoarthritis of the shoulder. All injections at Complete are performed using ultrasound guidance. Using the highest level of evidence-based treatment available will result in the most effective reduction in your symptoms possible. We do not require a GP referral. If you would like more information or would like to book an appointment please contact us on 0207 4823875 or email injections@complete-physio.co.uk.
What is injected during a shoulder injection for osteoarthritis?
Evidence suggests two injection techniques are clinically effective at significantly reducing pain and increasing function in shoulder osteoarthritis.
Ultrasound-guided corticosteroid injection
During this technique, a small dose of corticosteroid medication (a powerful anti-inflammatory drug regularly used in injection therapy) is mixed with a short-acting local anaesthetic. This is then injected, under guidance, directly into the affected shoulder joint. Corticosteroid is an effective pain-relieving medication and can take up to 2 weeks to reach its full potential. It is therefore advised that a short period of rest should be taken immediately after the injection to allow the corticosteroid to take effect.
Ultrasound-guided hyaluronic acid injection
Hyaluronic acid is a synthetic replica of the joint’s natural lubricant (synovial fluid). Hyaluronic acid has been proven to have both anti-inflammatory and analgesic effects and is capable of producing pain relief when injected into the osteoarthritic shoulder joint (Colen et al, 2014). Hyaluronic acid injections are regularly used as an alternative to steroid injections with good effect.
If you would like more information or would like to book an appointment please contact us on 0207 4823875 or email injections@complete-physio.co.uk.



Leave A Comment