What is a proximal hamstring tendinopathy?
The hamstring muscles attach, via a tendon, to the ischial tuberosity (the bones you sit on, deep to your buttock muscles). This tendon is called the proximal hamstring tendon. If this tendon is subjected to repetitive stresses and strains then the internal structure of the tendon can become comprised. Once compromised the affected tendon becomes weakened and can be painful. This is known as a proximal hamstring tendinopathy.
What are the symptoms of a proximal hamstring tendinopathy?
Symptoms of a proximal hamstring tendinopathy include:
- A sharp or deep aching pain located deep to the buttock over the sitting bone
- Pain which is made worse with prolonged sitting, standing after sitting, walking and exercise
- Latent pain deep to the buttock after exercise which can persist into the next day
- Pain that gradually increases after starting a new activity, often without trauma
- Pain when stretching your hamstring muscles
What other pathologies can present like a proximal hamstring tendinopathy?
- Femoroacetabular impingement
- Greater trochanteric pain syndrome
- Iliopsoas tendinopathy/bursitis
- Osteitis pubis
- Hip osteoarthritis
Proximal hamstring tendinopathy vs greater trochanteric pain syndrome
Both proximal hamstring tendinopathy and greater trochanteric pain syndrome are predominantly tendon related issues and are often associated with weak muscles around the hip. The key differentiating diagnostic factor is the location of pain. A proximal hamstring tendinopathy is felt deep to the buttock in contrast to the pain of greater trochanteric pain syndrome which is felt on the outer aspect of the hip.
What is proximal hamstring tendinopathy?
Tendinopathy of the proximal hamstring tendon is a common cause of buttock pain which can result in high levels of pain and disability. Tendon pathology is common in both occupational medicine and sport and is often associated with unaccustomed activity and overuse. Tendinopathy is believed to be responsible for up to 50% of injuries (Rees at al, 2009).
Proximal hamstring tendinopathy is a condition seen in patients of all ages from the young long-distance runners and sprinters to the more sedentary elderly person. It is also known as high hamstring or hamstring origin tendinopathy. The injury occurs at the attachment of the hamstring muscles onto the ischial tuberosity (your sitting bone).
It typically causes pain at the top of the leg (see image above) and will often begin at the buttock crease and refer down the leg. It is classically aggravated by sitting, prolonged walking, driving and running. Often patients have had this condition for several months or even years before we see them. It is known to be a difficult, frustrating injury to resolve.
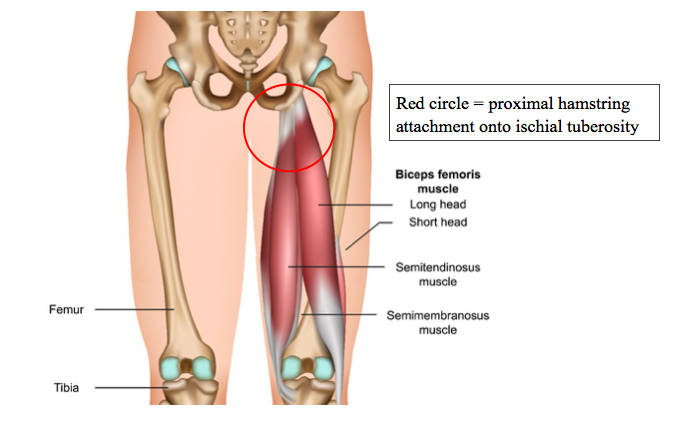
The anatomy of the hamstring
The hamstrings are a group of three muscles that are located at back of the thigh. These muscles are called the biceps femoris, semimembranosus and semitendinosus muscles. All of these muscles attach onto the ischial tuberosity (sitting bone) via a short, thick and powerful tendon (see image below). This is called the proximal hamstring tendon.
The hamstrings are a large powerful muscle group that are responsible for extending your hip and flexing your knee. They are under constant pressure during sport particularly running and sprinting and can become susceptible to pain and injury.
Why does proximal hamstring tendinopathy occur?
The exact cause is unknown but would appear to be related to repetitive strain and overload of the tendon.
The proximal hamstring tendon stores energy during activities such as running and jumping. When the tendon is subjected to excessive, high energy demands over a prolonged period of time, injury can occur. It is believed that tendon overload drives structural change within the tendon resulting in weakness and pain.
More specifically the excessive, high energy demand often occurs because you ramp up training too quickly and/or have insufficient recovery time between bouts of intense activity. For example, running everyday or playing football on a Saturday and Sunday, particularly if it is a new activity or you have not carried it out for a long period of time. Such activity may cause the tendon to become irritated and inflamed. This is called tendinitis.
Frequent episodes of tendinitis cause a sub-optimal healing process and the tendon becomes thickened and swollen. A thick, swollen tendon is known as being ‘tendinopathic’. This process can occur over months, but the actual pain often comes on quite quickly e.g. during a run.
On occasion you may have a specific injury to the tendon which causes a tear. This can occur during a sprint, reaching for a ball in football or stretching the hamstring beyond its limit e.g. carrying out the splits. Tears will often heal if they are given enough time, but it is not uncommon that you develop chronic tendon pain following a tear.

How is a proximal hamstring tendinopathy diagnosed?
Obtaining a correct diagnosis is essential for the implementation of the most effective treatment plan for your condition.
A formal diagnosis of proximal hamstring tendinopathy involves both a clinical assessment and diagnostic imaging. All clinicians at Complete are experienced physiotherapists and musculoskeletal sonographers so we can assess your injury using clinical tests and at the same appointment carry out a diagnostic ultrasound scan. A scan will confirm a diagnosis and also assess:
- Which tendons are involved?
- Is there a tear of the tendon?
- Is there any associated ischial bursitis?
- What is the severity of tendinopathy?
During your initial assessment we will also carry out a full assessment of your lower limb to identify any other potential contributing factors. This will include assessment of your muscle strength, flexibility and range of movement. During your assessment you may be asked to replicate the movement that instigates your pain. This might be performing a squat or running on a treadmill.
Once a diagnosis has been confirmed an individualised treatment plan will be designed.
What else could it be?
There are other conditions that can mimic proximal hamstring tendinopathy. These include:
- Referral from the lower back
- Irritation of the sciatic nerve (‘sciatica’)
- Sacro-iliac joint pain
- Posterior pubic or ischial ramus stress fracture
- Ischial femoral impingement
- In adolescents – apophysitis or avulsion
At your appointment we will be able to differentiate between these conditions. On occasion you can have more than one issue that is contributing to your pain. For example, it is not uncommon to have a proximal hamstring tendinopathy and irritation of the sciatic nerve.
How do we treat proximal hamstring tendinopathy?
Most people respond well to conservative management strategies. Physiotherapists often use a combination of manual soft tissue techniques and a progressive loading/rehabilitation program to strengthen the tendon and the muscle.
It is important to be aware that many tendon complaints are slow to improve and often take several months to improve. If you have had a tendon problem for over 6 months you should expect it to take 3 months to fully resolve. Rehabilitation is lengthy and takes both patience and persistence.
The good news is you rarely have to rest from all sports and activities. Rest has not been shown to be an effective treatment option for most tendinopathies including proximal hamstring pain.
Specific advice and rehabilitation will be provided after your assessment. However, here are a few quick tips that might help you on your path to recovery;
- Avoid or modify activities that cause pain. Common painful activities include running, cycling, squatting or deadlifting. For example, if you get pain with a 10-mile run try and modify your run to two 5 mile runs per week with 2-3 days recovery between them.
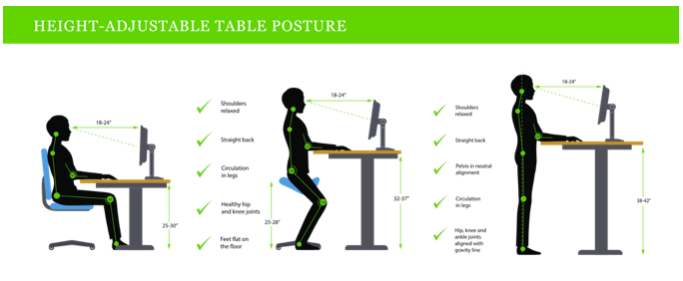
- Avoid aggravating postures. Limit long periods of sitting, particularly on a hard surface which can cause the tendon to become irritated. Crossing your legs can also put more pressure on the tendon.
- Use higher seats with a soft surface or use a standing desk. Some people like to sit on a blow-up doughnut cushion to avoid direct contact between the proximal hamstring tendon and the seat surface.
- We often find that stretching your hamstring can actually aggravate the pain. This causes compression on the tendon. Avoid stretches unless your clinician has advised you otherwise. If you carry out Yoga, it is likely you will need to modify your poses to ensure you do not aggravate the tendon.
- Start some gentle hamstring strengthening exercises. A good example is a bridging exercise (see image below). This can be started with both legs and then progressed to single leg bridges. Ideally you would lift your hips up and down slowly repeating 12 repetitions. Repeat three sets every other day.

What do you do if these strategies are not working?
Occasionally conservative management is not enough to resolve a proximal hamstring tendinopathy. In this case there are a few further treatment options available for you. These will be discussed with you by your clinician who can advise which is most appropriate for you following your assessment and ultrasound scan.
At this point there are two options:
- Shockwave therapy
- Ultrasound guided injection
Both options are an adjunct to treatment. This means they should not be seen as a stand-alone treatment but used alongside rehabilitation and activity modification.
Extracorporeal Shockwave Therapy
Shockwave therapy is an evidence-based treatment modality commonly used for treating tendon pain. This treatment option is designed to deliver a small amount of controlled micro-trauma to the affected tendon. This micro trauma initiates your natural healing process. Additionally, shockwave desensitises local nerve endings causing a reduction in pain. This can provide a window of opportunity to progress with your rehabilitation regime.
The research shows that shockwave is superior to physiotherapy and medication (NSAID’s) at 6 weeks and 12 months. This shows a long term positive on proximal hamstring tendinopathy pain (Cacchio et al, 2011).
The studies suggest between 3 to 5 shockwave sessions are required to reduce pain and improve the quality of your tendon. All of our clinicians are fully qualified to deliver shockwave treatment and have extensive experience using shockwave specifically for proximal hamstring pain.
Your clinician will inform you if this treatment modality is suitable for you. If you would like more information concerning shockwave therapy please contact us on 0207 4823875 or email injections@complete-physio.co.uk.
Ultrasound guided injection (USGI)
In a small percentage of proximal hamstring tendinopathy cases conservative management fails to resolve symptoms. If symptoms continue, we may discuss the role of steroid injections with you. Steroid is a strong anti-inflammatory.
Steroid injections are used for many tendon complaints and will help relieve inflammation and pain allowing you to progress with your rehabilitation program. In a majority of cases they significantly improve your sitting tolerance.
Steroid injections are not curative but again provide a window of opportunity to strengthen muscle and tendon in a pain free environment and allow you to return to your chosen activity.
Injections for the proximal hamstring tendinopathy must be carried out using ultrasound guidance. At Complete injections all our injections are carried out using real time ultrasound to guide the technique. We usually combine local anaesthetic with the steroid to reduce any pain associated with the procedure. We would expect you to get rapid pain relief from the injection. Most patients get a reduction in their pain 3-4 days following the injection. We always encourage you to start your rehabilitation exercise as soon as you experience the pain relief.
How many injections can you have?
We often get asked how many injections it is safe to have. In the case of proximal hamstring tendinopathy, it is very rare you will require more than one injection.
You should consider a steroid injection for proximal hamstring tendinopathy if:
1. You are unable to engage in a rehabilitation programme due to pain
2. Your quality of life is affected by the pain and you have not improved with conservative treatment e.g. physiotherapy
3. Your ability to sit is severely affected (less than 20 mins) and you have not improved with conservative treatment e.g. physiotherapy
All of our clinicians are fully qualified injection therapists and independent prescribers. Your clinician is able to prescribe the most appropriate medication and administer the injection under ultrasound guidance. If you would like more information regarding ultrasound guided contact us on 0207 4823875 or email info@complete-physio.co.uk.


Leave A Comment