Insertional Achilles tendinopathy is a common musculoskeletal complaint involving pain localised around the heel.
The incidence of Achilles tendon pain is approximately 6% in the general population, and 24% of people suffering from heel pain were diagnosed with insertional Achilles tendinopathy (Chimenti et al., 2017; Maffulli et al., 2020).

What is insertional Achilles tendinopathy?
Common signs and symptoms of insertional Achilles tendinopathy are:
- Pain and/or stiffness around the heel area first thing in the morning and especially when going downstairs.
- Pain and/or stiffness around the heel area when getting up after sitting for a prolonged period.
- Pain and/or stiffness when you initially start walking/running which may gradually ease.
- Swelling around the heel area.
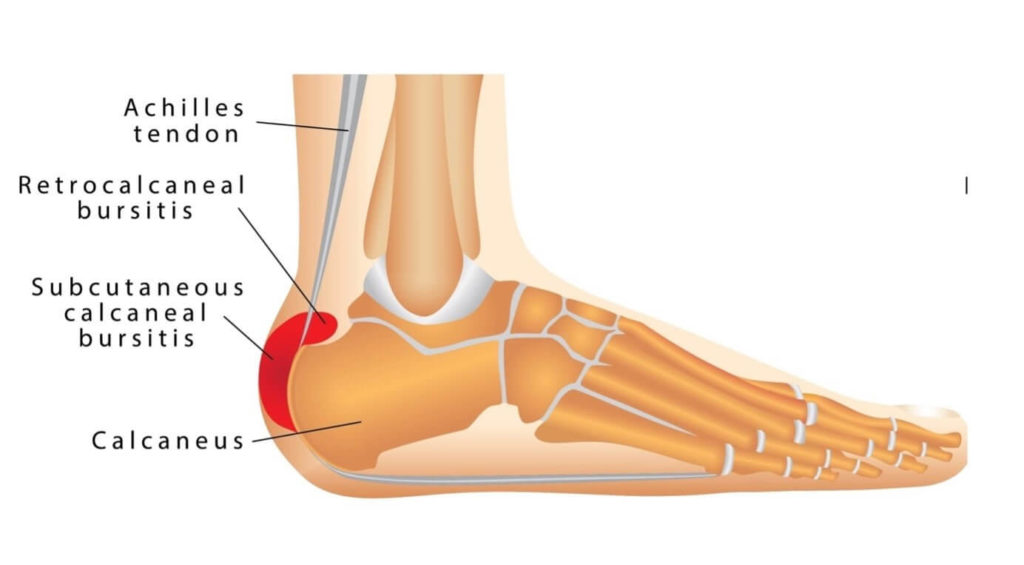
There are various structures which can contribute to insertional Achilles tendinopathy pain:
- Achilles tendon
- Calcaneus (heel bone) – with a Haglund’s deformity
- Subcutaneous calcaneal bursa (also known as superficial or pre-Achilles bursa)
- Retrocalcaneal bursa
- Kager’s fat pad
How do you diagnose insertional Achilles tendinopathy?
Clinically it is very hard to differentiate between the 5 structures around the Achilles insertion area and accurately identify the source of insertional Achilles tendinopathy symptoms. The use of diagnostic ultrasound is the best way to initially identify the structures and allow us to determine which of them could be contributing to insertional Achilles tendinopathy.

Bleakney and White (2005) recognised the benefits of diagnostic ultrasound, as it allowed clinicians to identify the two bursae (subcutaneous calcaneal bursa & retrocalcaneal bursa) which can be seen around the area of insertion of the Achilles tendon onto the calcaneus (heel bone). See image below
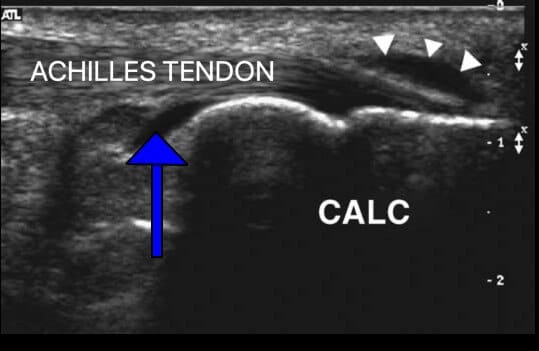
The retrocalcaneal bursa (blue arrow) lies deep to the Achilles tendon sitting between the Achilles tendon and the calcaneus. This bursa is commonly seen in normal (asymptomatic) subjects and varies considerably in appearance and size (Mathieson et al., 1988).
The subcutaneous calcaneal bursa (white arrowheads) is an “acquired” bursa that appears between the tendon and skin. This bursa is not seen in normal individuals; typically, it’s appearance on an ultrasound scan is normally only present after an injury or from an inflammatory condition (Frey, 1982).
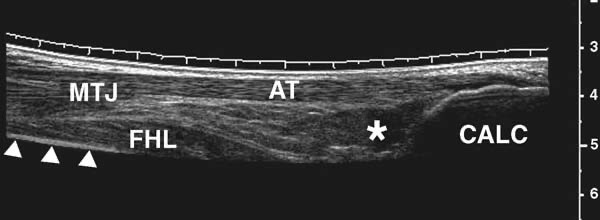
Additionally, Bleakney and White (2005) identify Kager’s fat pad (white star) lying below the Achilles tendon close to the calcaneal insertion. See image below.
An enlargement of the calcaneal tuberosity which may impinge against the Achilles tendon. Ultrasound imaging is found to be as good if not superior to MRI in identifying the presence of bony defects such as a Haglund’s deformity (Chimenti et al., 2016).
Finally, diagnostic ultrasound can be used to measure the thickness of the Achilles tendon, which should be approximately 6mm. Thickening seen and measured on diagnostic ultrasound is indicative of tendinopathy.
At Complete, clinical specialist physiotherapists will carry out an ultrasound as part of your assessment.
What are the treatment options for insertional Achilles tendinopathy?
The information we can gain from an ultrasound scan is essential to optimise your treatment. There are various management options available for insertional Achilles tendinopathy.
Initial management would include offloading the Achilles insertion by placing a heel wedge/lift in your shoe and choosing more appropriate footwear to limit any compression in that area.
Additionally, you could take some regular non-steroidal anti-inflammatory drugs (NSAIDs) and/or painkillers (eg. paracetamol).
Physiotherapy
If insertional Achilles tendinopathy symptoms persist, further management would include physiotherapy rehabilitation in the form of tendon loading.
It has been demonstrated for most Achilles tendon issues that heavy strength training is effective in alleviating symptoms.

Fahlstrom et al. (2003) however noted that it is very important to be aware of the negative effects of loading over a step for insertional Achilles tendinopathy as this could considerably aggravate patients’ symptoms by the fact that the calcaneal bone might be pressing on a chronically inflamed bursa and/or tendon.
This is in contrast to mid-portion Achilles tendinopathy where dropping over a step would not be provocative.
Most patients should undertake a tendon loading programme, ideally following these general principles:
- Low repetition – around 3 sets of 8 repetitions of each exercise
- High weight – the effort level needs to be very high, around 8/10
- Slowly – the longer the tendon is under tension the better
- Frequency – undertake the program 3 times per week
- Duration – the loading program needs to last for around 12 weeks
Shockwave
Alongside physiotherapy, extracorporeal shock wave therapy (ESWT) can be effective in helping reduce insertional Achilles tendinopathy symptoms.
Faria et al. (2017) demonstrated a positive effective in the use of ESWT alongside physiotherapy exercises in patients with insertional Achilles tendinopathy. These positive results were still present at 12 months after the treatment and were superior to physiotherapy alone.
The use of ESWT was further supported by Zhang et al. (2020), who showed ESWT can improve the symptoms of patients with insertional Achilles tendinopathy even at 5-year follow-up.
Injections
Unfortunately, some patients don’t respond to physiotherapy and ESWT, and in these cases an injection may be considered as a last option of treatment.
Injections however are designed to be carried out alongside your rehabilitation exercises and are not stand-alone treatments. Complete clinicians would discuss the pros and cons of any injection around a weight bearing tendon.
For insertional Achilles tendinopathy the purpose of an ultrasound guided injection is to alleviate any symptoms from:
- Subcutaneous calcaneal bursitis
- Retrocalcaneal bursitis
Using diagnostic ultrasound helps identify and correctly target and ensure the injection avoids the Achilles tendon, as we do not recommend injections to be carried out into the tendon itself.
For more information or to book a physiotherapy appointment, please call the number 020 7482 3875 or email info@complete-physio.co.uk.


