What is Tennis leg?
The calf (the muscles at the back of the lower leg) is formed by two muscles, the gastrocnemius and the soleus. A tennis leg refers to a tear of the connective tissue between these two large muscles. A tennis leg most commonly occurs on the inner (medial) aspect of the calf between the medial gastrocnemius and the soleus. A tennis leg is a very common injury and is associated with sudden high force trauma to the calf such as during a quick sprint or jump during sport or even, after an unexpected, quick calf stretch such as misjudging a step. A tennis leg can happen to anyone at any age however, the highest reported incidence rates are found within the sporting population and in middle aged men.
What are the symptoms of tennis leg?
- A sudden sharp pain in the calf muscle. Often felt immediately after a sudden movement.
- You might hear a popping sound in the calf at the time of the incident.
- Pain when you touch the calf muscles.
- In cases of significant tearing the calf muscle may change shape.
- Pain during walking that causes you to limp.
What other conditions can present as a Tennis leg?
Tennis leg vs Achilles tendinopathy
Location of pain is a key diagnostic factor between these conditions. A tennis leg is felt much higher up the calf in the muscle belly, whereas Achilles tendinopathy is felt on or just above the heel bone in the tendon. Tennis players leg causes tenderness in the calf muscle, whereas Achilles tendinopathy causes tenderness when you squeeze the Achilles itself. An Achilles tendinopathy is usually slow to build and is not associated with a traumatic event. This is in contrast to a tennis leg which occurs after a sudden quick movement.
Anatomy of the calf
Tennis leg refers to an injury of the calf muscle, more specifically the medial gastrocnemius muscle and the aponeurosis (connective tissue junction) between the medial gastrocnemius and the deeper soleus muscle of the calf.
The gastrocnemius originates from the femoral condyles of the femur (large bony prominences at the end of the long bones of the thigh) just above the knee, The muscle has two heads; the lateral head and medial head. The soleus muscle is the largest muscle of the calf complex and sits in front (deep to) the gastrocnemius.
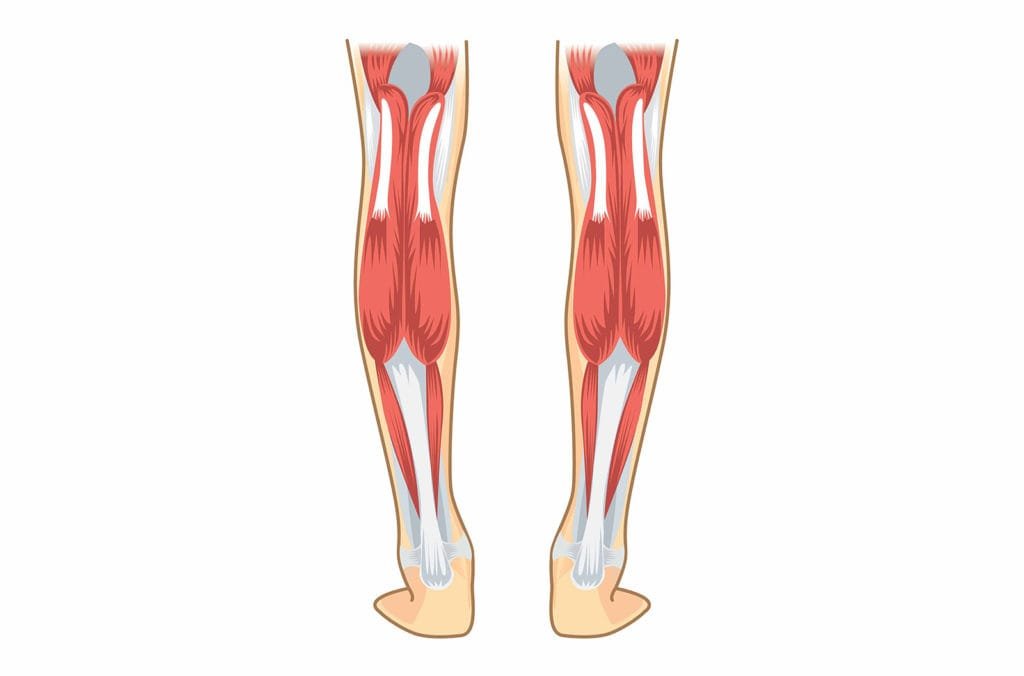
The lateral and medial head of the gastrocnemius and the soleus muscle converge to form the Achilles tendon, a common area of pain. The Achilles tendon inserts into the heel bone (calcaneus). The gastrocnemius is a powerful muscle that is used for dynamic and explosive movements, such as running and jumping. It is also involved in walking and standing activities but to a much lesser extent (Prakash et al., 2017).
The soleus muscle is a broad flat muscle that lies underneath the gastrocnemius. This is a powerful muscle which provides postural control and is the primary muscle used during walking (Prakash et al., 2017).
A calf muscle tear or tennis leg is the third most commonly treated muscle injury of the lower limb. Only being superseded by injuries to the bicep femoris (outer portion of hamstring muscle) and the rectus femoris (large powerful muscle of the thigh) (Domeracki et al., 2018).
How does a tennis leg injury occur?

Tennis leg is a traumatic, high force calf injury. Bright et al (2017) states that two thirds of all tennis leg injuries occur at the junction between the medial head of the gastrocnemius and the underlying soleus muscle. A tennis leg refers to a partial or complete rupture of the fascial attachment between these two muscles. The remaining one third of tennis leg injuries occur either at the lateral head of the gastrocnemius or within the belly of the gastrocnemius muscle itself.
A tennis leg can occur after small innocuous movements such as stretching the calf or walking however, most commonly occurs after a quick, explosive movement, when the knee is rapidly extending (straightening) during the pushing off phase of running or jumping (Domeracki et al., 2018). During this action the gastrocnemius muscle is subjected to the high forces and can fail, resulting in a tennis leg injury.
Although tennis leg is regularly observed within the sporting population research has revealed that tennis leg has its highest occurrence rates in poorly conditioned men over 40 years old (Bright et al., 2018).
How do you know if you have tennis leg?

Symptoms associated with tennis leg occur rapidly and cause immediate and significant pain.
Domeracki et al (2018) describes the typical presentation:
Symptoms of a calf tear (tennis leg) include:
- Sudden pain located in the calf
- An audible popping sound emanating from the calf
- Localised pain over the medial gastrocnemius when palpated (touched)
- If a full rupture has occurred, the muscle bulk of the calf may change shape
- Significant pain affecting ability to walk, resulting in a limp
How do we diagnose a calf tear (tennis leg)?
Diagnosis of tennis leg requires a diagnostic ultrasound scan as well as a clinical assessment.
A clinical assessment at Complete will include:
1. Clinical interview
To help formulate a hypothesis of tennis leg the clinician will ask a series of questions to understand how and why your pain started. A medical history will also be taking to rule out other causes for your pain including deep vein thrombosis (DVT). Differentially diagnosing a DVT is of critical importance as DVT requires urgent medical assistance, involving anticoagulant medication.
Physical assessment is used to locate the source of your symptoms and why they may have occurred. It includes:
- Close observation of the calf muscle for increased heat, swelling, bruising or calf muscle shape change (indicative of rupture)
- Ankle and calf range of movement
- Calf strength testing – can you stand on one leg or perform a heel raise?
- Gentle palpation (feeling) of the calf complex
- Walking assessment
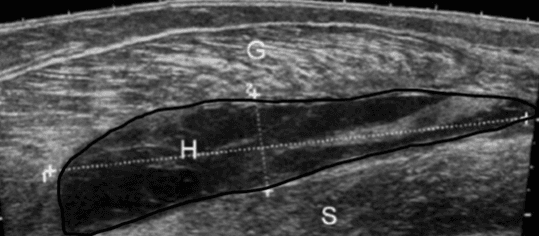
3. Diagnostic musculoskeletal ultrasound scan
Diagnostic musculoskeletal ultrasound imaging is the best imaging modality for a calf muscle tear. It visualises the injury better than an MRI scan and also provides information regarding whether or not there is a large haematoma (fluid collection – see image below) in the calf (a common occurrence in this injury). On your first appointment at Complete we will carry out a scan (no extra charge) and will determine whether the fluid should be aspirated (drained) to help with pain levels and the healing of the tear (more later).
Bright et al (2018) describe diagnostic ultrasound as capable of assessing the presence of calf injury, estimate the degree of severity and aid in its management by routinely monitoring the healing process throughout rehabilitation.
Timely completion of a diagnostic ultrasound scan is instrumental in providing an early onward referral for more focused DVT investigations if deemed appropriate (Bright et al., 2018).
If you would like more information or would like to book an appointment please contact us on 0207 4823875 or email injections@complete-physio.co.uk.
How do we treat tennis leg?

Tennis leg is routinely treated conservatively, under the management of a physiotherapist. Most patients respond well to physiotherapy with resolution of symptoms and return to exercise in 6-12 weeks depending on the extent of the tear.
Physiotherapy intervention often includes:
- Advice on activity modification – a short period of rest on the muscle from activities which aggravate your symptoms is highly recommended to avoid further injury and allow the healing process to occur.
- Pain management may include rest, ice, compression and elevation.
- Progressive weight-bearing advice – a crutch may be required during the initial stages to reduce pressure on the healing tissue and allow appropriate healing to occur.
- Gentle stretching exercises is avoided initially but will be introduced when appropriate by your physiotherapist depending on the extent of your injury.
- Progressive strengthening exercises for the calf muscles.
- Balance and stability exercises.
- Soft tissue techniques may be used to reduce pain and aid the healing process.
The above options will be discussed with you once you have had a diagnostic ultrasound scan carried out to assess the full extent of the injury.
Ultrasound guided aspiration (draining the haematoma/swelling)
As discussed earlier, fluid collections can accumulate between the gastrocnemius and soleus muscles. This can occur due to bleeding of the torn muscle fibres and surrounding connective tissue and is often known as a haematoma. The presence of a haematoma can significantly affect recovery times and cause a significant amount of pain and discomfort.
In some cases, we will suggest aspirating the fluid collection (hematoma) using ultrasound guidance. This is a straight forward, quick and relatively painfree procedure and will have a significant positive impact on your pain and recovery.
Patients regularly report significant reductions in pain immediately after the aspiration and are able to walk with less pain. The aspiration is followed up with a few days of compression and relative rest. To achieve maximum benefits, Complete recommend a course of physiotherapy starts 5-7 days post aspiration.
All clinicians at Complete are highly experienced at performing ultrasound-guided aspiration techniques. You are able to self-refer directly into our service without the need of a referral from doctor. If you would like more information or would like to book an appointment please contact us on 0207 4823875 or email injections@complete-physio.co.uk.


Leave A Comment