What is hyaluronic acid?
Articular cartilage is the smooth, low friction, shock absorbing structure covering the internal surfaces of a joint. The synovial membrane is the innermost lining of the joint capsule responsible for the production of synovial fluid, the joint’s natural lubrication. Both the articular cartilage and the synovial membrane are richly supplied with hyaluron receptor cells. Hyaluronic acid readily binds to hyaluron receptor cells where it acts as a semi-permeable membrane between the synovial fluid and the articular cartilage, providing joint lubrication and shock absorption (Sirin et al., 2018). Effective joint lubrication is dependent on the viscoelastic properties of hyaluronic acid. Viscosity is, in turn, directly related to the molecular weight of hyaluronic acid. A reduction in the molecular weight of hyaluronic acid lowers its viscosity resulting in a poorly lubricated joint, reduced ability to absorb shock, and ultimately osteoarthritic joint changes (Bowman et al., 2018).
Hyaluronic acid demonstrates a series of rheological properties. It primarily acts as a joint lubricant. However, due to its highly viscous structure, it supports the joint space allowing for additional shock absorption. Furthermore, hyaluronic acid regulates protein synthesis and acts as a scavenger of free radicals. Free radicals are highly reactive, unstable cells capable of causing pathological disease processes within a joint (Ziskoven et al., 2010).
What is hyaluronic acid made of?
Traditionally hyaluronic acid was prepared using rooster combs (the fleshy crest located on the top of the head of male birds such as chickens and pheasants). However, this has now been widely replaced by a process called bio-fermentation. Bio-fermentation uses specific bacteria cultures to produce a synthetic hyaluronic acid solution. Bio-fermentation has a higher safety profile and is more cost effective than hyaluronic acid prepared using rooster combs and therefore is now the preferred production method.
How does intra-articular hyaluronic acid therapy (IAHA) work?
The mechanism of action of IAHA has been well documented over the last decade. Research has revealed that the introduction of IAHA into an osteoarthritic knee joint initiates a series of chemical chain reactions which provide chondroprotection (preventing chondrocyte death whilst encouraging the development of new articular cartilage) and lowers joint inflammation. IAHA has also been shown to provide an increase in joint lubrication and shock absorption (known as viscosupplementation), initiate the production of proteoglycans (proteins responsible for the development of soft tissues such as joint cartilage) and promote the development of subchondral bone growth (Altman et al., 2015; Cheng et al., 2014).
The plethora of chemical reactions associated with IAHA produces a series of disease modifying actions which have been shown to provide significant moderate to long term pain relief, increased function, improved quality of life and reduced joint stiffness (Maheu et al., 2019; Altman et al., 2015; Sirin et al., 2018; Gigis et al., 2016). In fact, research has suggested that repeated IAHA can postpone total knee replacement by up to 5 years (Maheu et al., 2019).
Altman et al. (2015) conducted a comprehensive systematic review to further understand the mechanism of action of IAHA. Findings from this extensive report revealed five main mechanisms of action attributed to IAHA. These complex biochemical processes are presented below:
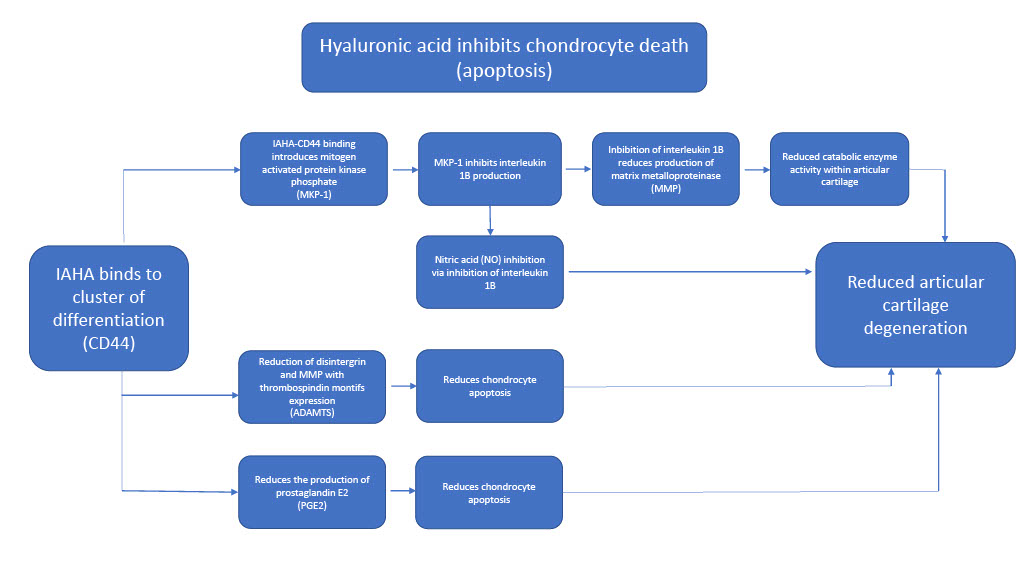
Mechanism of action 1 – chondroprotection.
Chondroprotection has been widely reported as the key attribute associated with IAHA. Chondrocytes, cells found within articular cartilage, are responsible for replenishing damaged tissue and maintaining the health of the articular cartilage. Chondroprotection is created by inhibiting chondrocyte death (apoptosis) whilst providing an environment capable of protecting existing chondrocytes.
Supplementary chondroprotection is achieved by the introduction of IAHA. Hyaluronic acid replacement, in the form of IAHA, binds to pre-existing hyaluron receptors within the synovial membrane and articular cartilage thereby restoring joint equilibrium.
The mechanism of action of IAHA is initiated by its binding to CD44 (cluster of differentiation) receptors. CD44 receptors are found on the surface of many cells including both hyaluronic acid and hyaluron cells (Senbanjo et al., 2017). The CD44-IAHA binding action produces a series of chemical chain reactions including the inhibition of chondrocyte apoptosis. The table below explains these processes in more detail.
Mechanism of action 2 – proteoglycan synthesis.
Proteoglycans are proteins found extensively throughout all connective tissue types, including articular cartilage. The dominant proteoglycan found within articular cartilage is known as aggrecan. Aggrecan hydrates the articular cartilage which in turn increases the swelling pressure within the tissue. Increased swelling pressure enables the articular cartilage to withstand higher compressive forces, an attribute essential for avoiding injury as well as maintaining the health of articular cartilage (Yanagishita, 1993). Hyaluronic acid has been reported to promote the production of aggrecan and because of this it has been suggested that IAHA may have the ability to strengthen the extra cellular make-up of the articular cartilage protecting it from further injury and degenerative change (Altman et al., 2015).
Mechanism of action 3 – production of anti-inflammatory mediators.
Interleukin – 1B and Prostaglandin E2 (PGE2) are two prominent pro-inflammatory mediators. CD44-IAHA binding inhibits the production of these inflammatory markers thereby reducing pain and inflammation (Altman et al., 2015; Sirin et al., 2018).
Mechanism of action 4 – increased joint lubrication and shock absorption.
As previously discussed, the viscoelastic properties associated with hyaluronic acid provides a joint with both lubrication and shock absorption. IAHA has also been shown to provide the knee joint with elevated levels of both these essential mechanical joint attributes (Altman et al., 2015; Sirin et al., 2018). Interestingly, IAHA has a residence time, within a knee joint, of only a few days and therefore the mechanical attributes of hyaluronic acid are not believed to be responsible for the long-term positive effects IAHA has on joint pain and function (Maheu et al., 2019).
Mechanism of action 5 – promotion of subchondral bone development.
Osteoarthritic joint changes disrupt the delicate interplay between subchondral bone osteoblast activity (cells responsible for the production of new bone) and chondrocytes found within articular cartilage. Once again, CD44-IAHA binding has been shown to stimulate an increase in the turnover of type 2 collagen at the interface between the subchondral bone and the articular cartilage resulting in an increase in subchondral bone density. Increased subchondral bone density increases its compliance, resulting in reduced pressure within the articular cartilage (Altman et al., 2015).
Are hyaluronic acid injections comfortable and safe to perform?
Hyaluronic acid has been shown to provide longer term pain relief and result in less side effects (cardiovascular and gastrointestinal) than oral non-steroidal anti-inflammatories (Sirin et al., 2018). Although IAHA produces longer lasting benefits when compared to corticosteroid injection, IAHA took much longer to take effect, with an average lead time of between 2 to 5 weeks (Gigis et al., 2016; Bowman et al., 2018).
Post injection pain flare is a potential post injection complication for both corticosteroid and IAHA injections, however evidence has shown that post IAHA injection pain flares typically only occur after repeated injections and are only very rarely documented. Post IAHA pain is believed to be due to the repeated accumulation of hyaluron breakdown products within the joint space as most reports of pain occur in patients undertaking multiple injections rather than individual IAHA procedures. Furthermore, bio-fermentation solutions provide a higher safety profile than IAHA produced using rooster combs (Altman et al., 2015).
To date and to the best of the authors knowledge there is no evidence suggesting any increase in post injection complications including infection, anaphylaxis, skin depigmentation or fat atrophy when compared to corticosteroid injections. In fact one study discussed by Maheu et al., (2019) reported only three reported post injection complications with one case being anaphylaxis in a sample population of 9214 patients.
Research has shown that intra-articular injections completed under ultrasound guidance are significantly more accurate, cause less post injection complications, and produce better outcomes than landmarked guided injections (Maricar et al., 2012). Furthermore, an IAHA injection performed under ultrasound guidance has been shown to be less painful than one administered without guidance (Lundstrom et al., 2019).
Are all hyaluronic acids created equal? Does molecular weight matter?
Hyaluronic acid is available as either low molecular weight (LMW), a molecular weight ranging between 80-800kDa or high molecular weight (HMW), a molecular weight of above 800kDa. The viscosity of hyaluronic acid directly effects its ability to bind to CD44 receptors and therefore the effectiveness of IAHA is intrinsically linked to its molecular weight (Rayahin et al., 2016; Altman et al., 2015; Mohebbi et al., 2021). Different molecular weight hyaluronic acid solutions have been observed to have varying physiological effects. LMW hyaluronic acid has been reported to possess greater chondroprotective capabilities than its HMW counterpart however, HMW hyaluronic acid is suggested to produce more anti-inflammatory effects (Huang et al., 2010).
However, is one molecular weight more effective than another? Theoretically speaking, it would seem logical to deduce that LMW would be superior to HMW due to the aforementioned significance of the chondroprotective mechanism of action associated with IAHA. However, what does the research conclude?
Evidence remains inconclusive as to which solution is clinically more effective, LMW or HMW. The current evidence, primarily based on osteoarthritis of the knee, uses a wide variety of methodologies to reach its conclusions and so gaining a consensus as to which solution is most efficacious is challenging.
A direct comparative study undertaken by Gigis et al. (2016) revealed no significant difference between HMW and LMW hyaluronic acid when treating knee osteoarthritis. High and low molecular weight hyaluronic acid were reported to be effective at reducing joint stiffness and pain and improving function. However, this study used a course of 5 injections over 5 weeks, a frequency of treatment not often clinically achievable. A systematic review conducted by Bowman et al. (2018) reported outcomes for both single and multiple IAHA injections and also reported no significant difference between HMW and LMW solutions for treating knee osteoarthritis. Interestingly, a single HWM IAHA injection has been reported to be as effective, for knee osteoarthritis, as multiple LMW IAHA injections, with positive benefits remaining for up to 6 months (Bahrami et al., 2020).
In conclusion, the current evidence supports the use of IAHA injections (for knee osteoarthritis). Both HMW and LMW solutions can produce equally positive outcomes. However, from a safety, time and cost saving prospective it, a single HMW IAHA injection would be preferable to multiple LMW IAHA injections.
What conditions can hyaluronic acid effectively treat?
As previously described, there is a rapidly growing body of evidence to support IAHA as an effective injection option within musculoskeletal healthcare. Most of the evidence base has been conducted in the field of osteoarthritis, in particular the knee. Research surrounding the efficacy of IAHA is constantly evolving and new evidence is continually being published. A brief description of the evidence, divided into conditions, is discussed below:
The knee
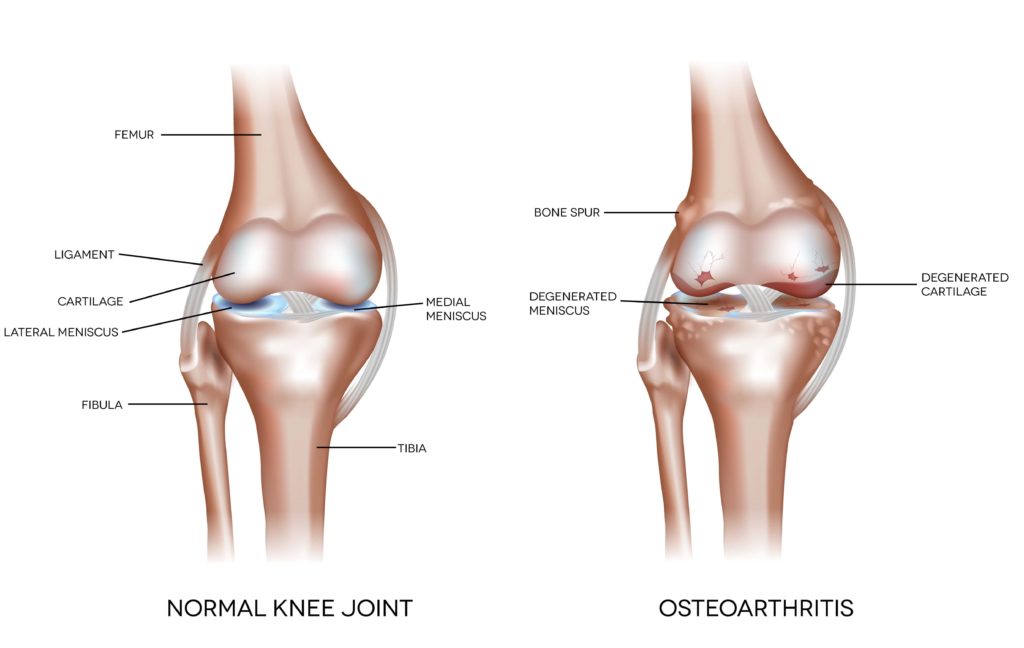
Evidence for the effectiveness of IAHA injections in knee OA management has been extensively documented. The current literature supports IAHA as a safe and effective method of controlling pain (for up to 6 months), reducing oral pain killer consumption, increasing function, increasing quality of life and delaying surgical intervention (Altman et al., 2015; Baron et al., 2018; Maheu et al., 2019; Gigis et al., 2016; Bahrami et al., 2020; Patakioutis et al., 2020). HMW IAHA has been shown to produce particularly effective results when treating knee osteoarthritis patients of working age (Hermans et al., 2019).
The hip
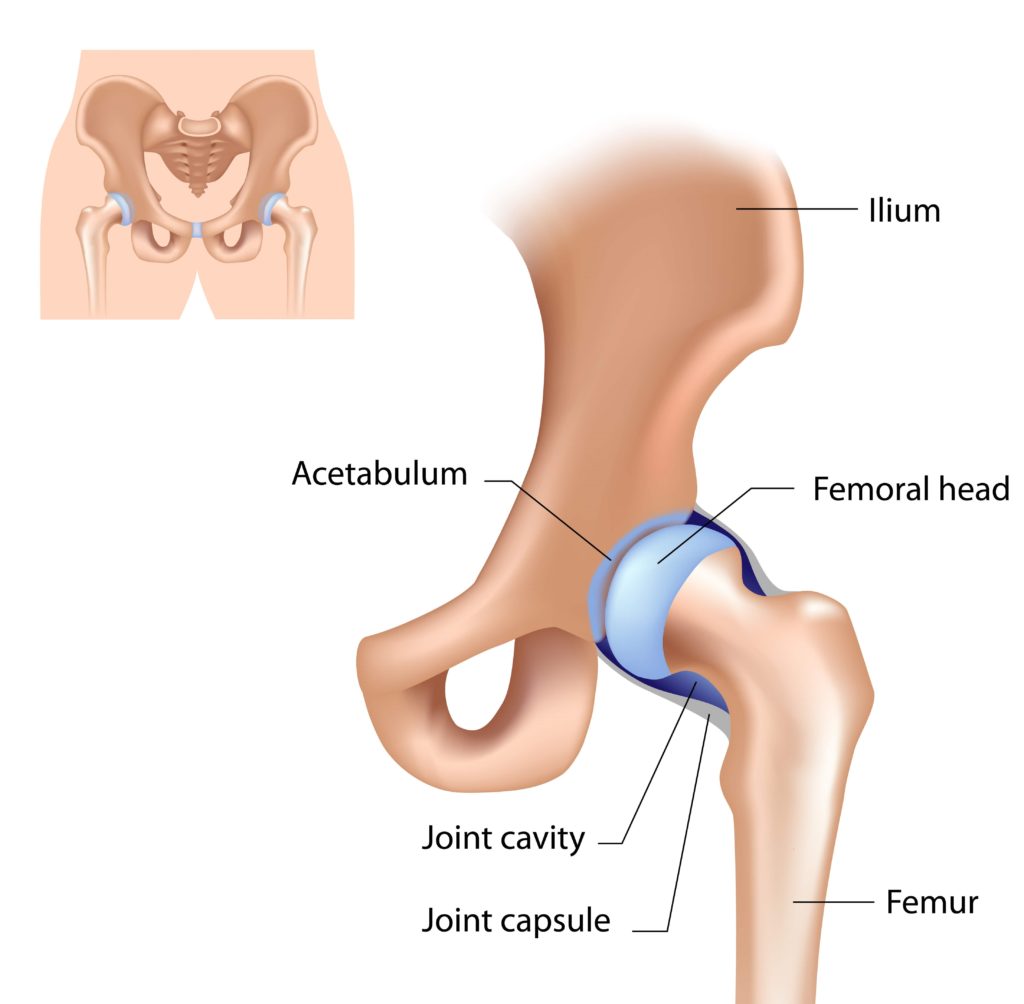
A large systematic review concerning IAHA and hip OA conducted by Wu et al. (2021) revealed that the efficacy of IAHA increased in line with the molecular weight of the product. Reduced pain and increased hip joint function were observed to last for up to six months post IAHA injection. Furthermore, adverse effects occurred only very rarely, supporting previous research. Research by Bowman et al. (2018) supports Wu et al. (2021), who also noted poorer IAHA outcomes with advancing osteoarthritic change.
Further research has also revealed that two IAHA injections, one week apart, had the ability to reduce pain, increase quality of life and improve functional ability in patients suffering from femoroacetabular hip impingement. These benefits were maintained for up to one year (Ometti et al., 2020).
The ankle

Current research is limited concerning the effectiveness of IAHA and ankle OA. The available literature does suggest that IAHA has favourable outcomes in both pain and function, but further research is required to confirm this (Vannabouthong at el., 2018). Significant reductions in pain associated with IAHA injections for ankle OA was also supported in a systematic review undertaken by Bowman et al. (2018) who further concluded that maximum gains could be achieved using a course of multiple IAHA injections.
Interestingly, IAHA has been proven to be a highly effective treatment modality for patients who have failed surgical correction for osteochondral ankle lesions. Three consecutive IAHA injections, one week apart, was shown to produce significant increases in function as well as significant reductions in pain. IAHA was postulated to be a safe and effective alternative to further surgical interventions for these patients (Hwang et al., 2020).
The shoulder
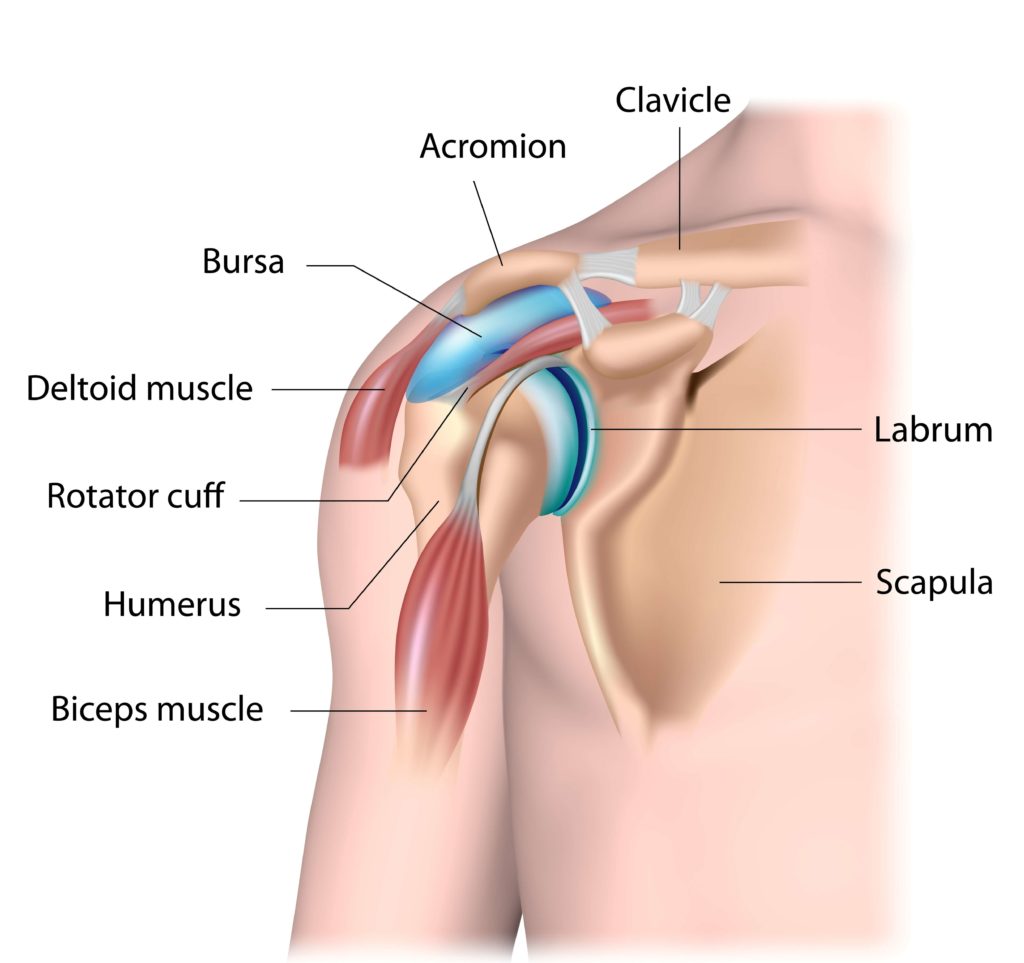
Once again, there is currently very little published research to support the effectiveness of IAHA for treating the shoulder. However, preliminary evidence is positive. A single IAHA injection targeting the sub acromial bursa of the shoulder has been shown to produce clinically significant pain relief, reduced disability and increased function for up to three months. These positive effects were observed to be partially sustained for up to six months. This research observed equal benefits for both HMW and LMW IAHA preparations, although LMW injections were reported to be better tolerated by patients and therefore LMW IAHA injections were recommended for treating rotator cuff pathology (Mohebbi et al., 2021).
The thumb

A systematic review discussing treatment options available for OA thumb reported IAHA injections significantly increased thumb function. However, corticosteroid injections were more effective at controlling pain (Trellu et al., 2015). This view has been supported by further work from Koh et al. (2019) who concluded IAHA to be an effective modality for treating thumb OA, but due to the delay in efficacy associated with IAHA injections a combination of IAHA and steroid was recommended.
How do we optimise the outcomes after a hyaluronic acid injection?

As previously discussed, hyaluronic acid has been shown to provide effective pain relief as well as increase quality of life and function in patients suffering from osteoarthritis. Maheu et al., (2019) noted that patients with the following attributes respond most favourably to IAHA injections;
- Mild to moderate osteoarthritis diagnosed on X-ray.
- Patients aged up to 60 years old respond most favourably to IAHA injections.
- Patients, of any age, who require regular multiple medications to manage pain levels.
- High levels of pain and symptoms.
- No evidence of knee joint swelling.
Furthermore, a course of physiotherapy is advised after an IAHA injection. The evidence surrounding the treatment and management of osteoarthritis clearly states that maintaining strength and flexibility of the affected joint as well as the supporting musculature plays a significant role in managing the progression of the condition (Hunter et al., 2009).

Conclusion
Research has shown hyaluronic acid to be an effective treatment choice for people suffering from osteoarthritis, in particular knee osteoarthritis.
Hyaluronic acid can provide significant reductions in pain, increases in quality of life, and improved functional ability in a variety of ways. The mechanisms of action of IAHA are complex and multi-factorial and including chondroprotection, the promotion of proteoglycan synthesis, elevating anti-inflammatory mediators, increasing joint lubrication and shock absorption and the development of subchondral bone.
The jury remains out as to which molecular weight solution is most beneficial, with both products achieving good clinical outcomes. Further research is required in this area to fully answer the question.
Due to the positive attributes of IAHA injections the American Medical Society for Sports Medicine (2015) promotes its use for patients suffering from knee osteoarthritis and in particular for those patients aged between 40 and 60 years of age with active lifestyles.
For more information about hyaluronic acid injections or to book a consultation, please call 020 7482 3875 or email info@complete-physio.co.uk
References
- Altman, R.D., Manjoo, A., Fierlinger, A., Niazi, F. & Nicholls, M. 2015, “The mechanism of action for hyaluronic acid treatment in the osteoarthritic knee: a systematic review”, BMC musculoskeletal disorders, vol. 16, no. 1, pp. 321.
- Bahrami, M.H., Raeissadat, S.A., Cheraghi, M., Rahimi-Dehgolan, S. & Ebrahimpour, A. 2020, “Efficacy of single high-molecular-weight versus triple low-molecular-weight hyaluronic acid intra-articular injection among knee osteoarthritis patients”, BMC musculoskeletal disorders, vol. 21, no. 1, pp. 550.
- Baron, D., Flin, C., Porterie, J., Despaux, J. & Vincent, P. 2018, “Hyaluronic Acid Single Intra-Articular Injection in Knee Osteoarthritis: A Multicenter Open Prospective Study (ART-ONE 75) with Placebo Post Hoc Comparison”, Current therapeutic research, vol. 88, pp. 35-46.
- Bowman, S., Awad, M.E., Hamrick, M.W., Hunter, M. & Fulzele, S. 2018, Recent advances in hyaluronic acid based therapy for osteoarthritis, Wiley.
- Chen, C.P.C., Hsu, C.C., Pei, Y., Chen, R.L., Zhou, S., Shen, H., Lin, S. & Tsai, W.C. 2014, “Changes of synovial fluid protein concentrations in supra-patellar bursitis patients after the injection of different molecular weights of hyaluronic acid”, Experimental gerontology, vol. 52, pp. 30-35.
- Hermans, J., Bierma-Zeinstra, S., Bos, K., Niesten, D., Verhaar, J. & Reijman, M. 2019, “The effectiveness of high molecular weight hyaluronic acid for knee osteoarthritis in patients in the working age: a randomised controlled trial”, BMC musculoskeletal disorders, vol. 20, no. 1, pp. 196.
- Huang, T., Hsu, H., Yang, K., Yao, C. & Lin, F. 2010, “Effect of Different Molecular Weight Hyaluronans on Osteoarthritis-Related Protein Production in Fibroblast-Like Synoviocytes From Patients With Tibia Plateau Fracture”, The journal of trauma, vol. 68, no. 1, pp. 146-152.
- Hunter, D.J. & Bierma-Zeinstra, S. 2019, “Osteoarthritis”, The Lancet, vol. 393, no. 10182, pp. 1745-1759.
- Hwang et al., 2020. Intra-articular Injections of Hyaluronic Acid on Osteochondral Lesions of the Talus After Failed Arthroscopic Bone Marrow Stimulation d, .
- Koh, S.H., Lee, S.C., Lee, W.Y., Kim, J. & Park, Y. 2019, “Ultrasound-guided intra-articular injection of hyaluronic acid and ketorolac for osteoarthritis of the carpometacarpal joint of the thumb”, Medicine, vol. 98, no. 19.
- Lundstrom, Z.T., Sytsma, T.T. & Greenlund, L.S. 2020, “Rethinking Viscosupplementation: Ultrasound‐ Versus Landmark‐Guided Injection for Knee Osteoarthritis”, Journal of ultrasound in medicine, vol. 39, no. 1, pp. 113-117.
- Maheu, E., Bannuru, R.R., Herrero-Beaumont, G., Allali, F., Bard, H. & Migliore, A. 2019, “Why we should definitely include intra-articular hyaluronic acid as a therapeutic option in the management of knee osteoarthritis: Results of an extensive critical literature review”, Seminars in arthritis and rheumatism, vol. 48, no. 4, pp. 563-572.
- Maricar, N., Callaghan, M.J., Felson, D.T. and O’Neill, T.W., 2013. Predictors of response to intra-articular steroid injections in knee osteoarthritis—a systematic review. Rheumatology, 52(6), pp.1022-1032.
- Mohebbi et al., 2021. High- Versus Low-Molecular-Weight Hyaluronic Acid for the Treatment of Rotator Cuff Tendinopathy b, .
- Ometti, M., Schipani, D., Conte, P., Pironti, P. & Salini, V. 2020, “The efficacy of intra-articular HYADD4-G injection in the treatment of femoroacetabular impingement: results at one year follow up”, Journal of drug assessment (London, U.K.), vol. 9, no. 1, pp. 159-166.
- Rayahin, J.E., Buhrman, J.S., Zhang, Y., Koh, T.J. & Gemeinhart, R.A. 2015, “High and Low Molecular Weight Hyaluronic Acid Differentially Influence Macrophage Activation”, ACS biomaterials science & engineering, vol. 1, no. 7, pp. 481-493.
- Sirin, D.Y., Kaplan, N., Yilmaz, I., Karaarslan, N., Ozbek, H., Akyuva, Y., Kaya, Y.E., Oznam, K., Akkaya, N., Guler, O., Akkaya, S. & Mahirogullari, M. 2018, “The association between different molecular weights of hyaluronic acid and CHAD, HIF-1α, COL2A1 expression in chondrocyte cultures”, Experimental and therapeutic medicine, vol. 15, no. 5, pp. 4205-4212.
- Senbanjo, L.T. & Chellaiah, M.A. 2017, “CD44: A Multifunctional Cell Surface Adhesion Receptor Is a Regulator of Progression and Metastasis of Cancer Cells”, Frontiers in cell and developmental biology, vol. 5, pp. 18.
- Sirin, D.Y., Kaplan, N., Yilmaz, I., Karaarslan, N., Ozbek, H., Akyuva, Y., Kaya, Y.E., Oznam, K., Akkaya, N., Guler, O., Akkaya, S. & Mahirogullari, M. 2018, “The association between different molecular weights of hyaluronic acid and CHAD, HIF-1α, COL2A1 expression in chondrocyte cultures”, Experimental and therapeutic medicine, vol. 15, no. 5, pp. 4205-4212.
- Trellu, S., Dadoun, S., Berenbaum, F., Fautrel, B. & Gossec, L. 2015, “Intra-articular injections in thumb osteoarthritis: A systematic review and meta-analysis of randomized controlled trials”, Joint, bone, spine : revue du rhumatisme, vol. 82, no. 5, pp. 315-319.
- Vannabouthong at el., 2018. Intra-articular Injections in the Treatment of Symptoms from Ankle Arthritis c, .
- Wu et al., 2021. Molecular Weight of Hyaluronic Acid Has Major Influence on Its Efficacy and Safety for Viscosupplementation in Hip Osteoarthritis A Systematic Review and Meta-Analysis e, .
- Yanagishita M. Function of proteoglycans in the extracellular matrix. Acta Pathol Jpn. 1993 Jun;43(6):283-93. doi: 10.1111/j.1440-1827.1993.tb02569.x. PMID: 8346704.
- Ziskoven, C., Jäger, M., Zilkens, C., Bloch, W., Brixius, K. and Krauspe, R., 2010. Oxidative stress in secondary osteoarthritis: from cartilage destruction to clinical presentation?. Orthopedic reviews, 2(2).


