What is patella tendinopathy (also known as Jumper’s knee)?
Patella tendinopathy is an overuse injury which causes pain and tenderness in the tendon at the front of the knee. The tendon connects the quadriceps muscles (thigh muscle) to the bone at the top of your shin (known as the tibia). It is aggravated by any activities that require a large contraction of the quadriceps muscle such as squatting, lunging and particularly impact activities such as hopping, jumping and running. Often the pain is better during activity and worse afterwards.
Diagnostic ultrasound is the gold standard imaging modality to diagnose a patella tendinopathy and to visualise if there is a tear. At Complete this is carried out at no extra cost during your first appointment.
Complete rest is not normally advised for patella tendinopathy. Stretches have also been shown to be of limited value in getting you back to sport. Physiotherapy, involving heavy slow resistance (HSR) training and activity modification, has been shown to be the most successful treatment for patella tendinopathy. Shockwave therapy alongside physiotherapy is also an effective treatment regime. If you are still struggling with pain having completed your physiotherapy and shockwave programmes, a high volume saline injection or a platelet rich plasma (PRP) injection are both potential options.
What are the symptoms of patella tendinopathy?
- Pain when you press the tendon at the front of the knee just below your knee cap
- Pain with impact activates such as running and jumping.
- Pain that reduces with activity and is often worse afterwards.
If this sounds like your problem, read on below…
Other conditions that are associated with a patella tendinopathy are:
- Cartilage (meniscal) tear
- Osteoarthritis of the knee
- Patellofemoral (knee cap) pain
- Prepatella bursitis
- Pes anserine tendinopathy
- Fat pad inflammation
Patella tendinopathy vs Patellofemoral (knee cap) pain
Patella tendinopathy normally gives specific localised pain at the front of the knee at the lowest aspect of the patella (knee cap) and is tender when you press the tendon. Whereas patellofemoral joint pain often gives rise to more diffuse (widespread) pain on the front of the knee with no obvious tender spots when you press the knee.
Patella tendinopathy pain is often worse after an activity, rather than during. Patellofemoral knee joint pain is normally worse during the activity and eases after the activity. Both conditions are aggravated by impact activities such as running and jumping and going downstairs.
What is patella tendinopathy?
Tendinopathy is believed to be accountable for a significant proportion of all musculoskeletal pathology resulting in referral to a health professional (Resteghini et al., 2016).
Patella tendinopathy, commonly known as jumper’s knee, is predominantly an overuse injury. The patellar tendon is subjected to high levels of stress via the action of the knee extensor mechanism. It is a common site for pain and injury to occur, especially among the sporting population. Research has shown patella tendinopathy to be present in up to 14-16% of all athletes who play sports requiring jumping, such as volleyball and basketball (Cong et al., 2016).
When the patellar tendon is subjected to regular episodes of high-intensity activity, often involving jumping, the tendon can become inflamed and painful. An inflamed and painful tendon is known as tendinitis. If the patellar tendon is repeatedly exposed to further episodes of tendinitis the tendon is unable to recover fully resulting in an incomplete, sub-optimal healing response. The result of incomplete tendon healing is a pathologically weak and thickened tendon. A weak and thickened tendon is known as a tendinopathy. A pathologically weak tendon can cause significant pain and disability and in severe cases can result in tears (Cong et al., 2016).
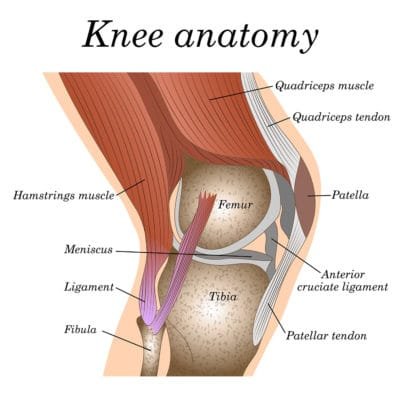
Anatomy of the patella tendon
The patella tendon is located between the bottom of your patella (kneecap) and the top of your tibia (long bone of the shin). The patella tendon is a continuation of the quadriceps tendon that is located just above the patella. It attaches to the large muscles at the front of your thigh called the quadriceps muscle (see the below image).
The quadriceps muscles, quadriceps tendon, patella and patellar tendon are responsible for extending (straightening) your knee during running and jumping and are collectively known as the knee extensor mechanism.
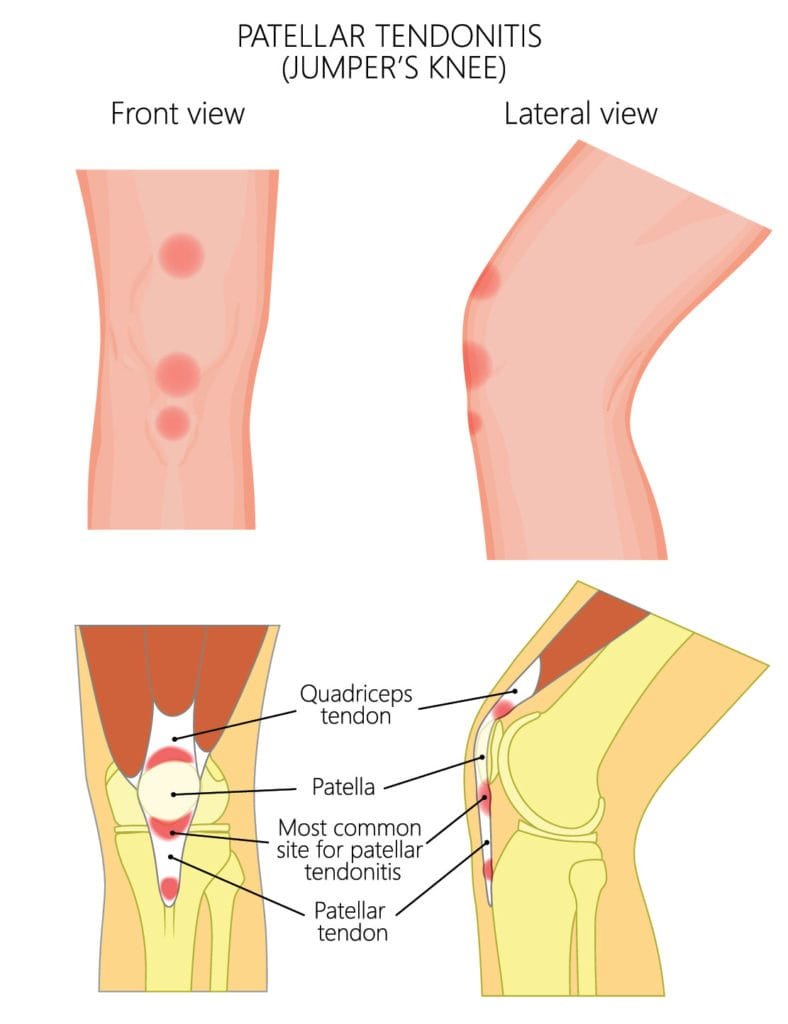
Jumper’s knee refers to tendinopathy at three specific locations within the knee extensor mechanism (Dan et al., 2018).
Dan et al. (2018) describe the following tendon pathologies (see below image) as associated with Jumper’s knee:
- Insertional quadriceps tendinopathy – the quadriceps tendon attaches to the uppermost aspect of the patella. Insertional quadriceps tendinopathy has been reported in 25% of all jumper’s knee cases.
- Proximal patella tendinopathy (also known as inferior pole tendinopathy) – the patella tendon originates from the bottom of the patella at a point known as the ‘inferior pole’. Proximal patella tendinopathy has been documented to account for 65% of all jumper’s knee pain. This is by far the most common cause we see at Complete.
- Distal patella tendinopathy (also known as tibial tubercle tendinopathy) – the patellar tendon inserts in a small bony prominence at the top of the tibia called the tibial tubercle, and this region is responsible for approximately 10% of all jumper’s knee cases.
This rest of this article focuses on the most common condition of the three; proximal patella tendinopathy.
Common risk factors associated with the onset of tendinopathy include:
- Sport involving repetitive, high intensity, knee extension such as running, squatting, climbing and jumping
- Age – tendinopathy is most commonly seen later on in life
- Sex – patella tendinopathy is most commonly seen in men
- Muscular imbalances can occur due to muscle weakness or tightness. This can change the biomechanics around the knee, resulting in patella tendon overload and tendinopathy.
- Inadequate preparation for sport – if you have not prepared your tendon for the increased demands required during sport it can be susceptible to injury. Sport specific strength training and an effective warm up is essential to prevent tendinopathy.
- Sudden changes in activity levels such as starting a new sport and increasing frequency or intensity of your exercise too quickly.
- Tendinopathy has also associated with increased weight (high body mass index (BMI)), high cholesterol, diabetes and other metabolic conditions.
How do we know if you have patella tendinopathy?
Symptoms of often present gradually, without trauma, and can take many months of repetitive overloading of the tendon before becoming problematic.

Symptoms of patella tendinopathy include:
- Pain located just below the knee cap
- Pain which is made worse with increased levels of activity such as walking, running or jumping.
- Pain is often worse after activity
- Pain after prolonged periods of rest such as when rising from sitting at your desk or from getting out of bed in the morning.
- Pain with negotiating stairs and inclines.
- Morning stiffness – your knee may feel stiff first thing in the morning. Stiffness typically wears off within an hour.
How is patella tendinopathy diagnosed?
Obtaining an accurate diagnosis of jumper’s knee is essential. It allows the clinician to select the most effective treatment plan for you. A diagnosis will be made by your clinician by carrying out a comprehensive clinical assessment and a diagnostic ultrasound scan.

Clinical assessment regularly includes the following:
- An in-depth clinical interview – your clinician will ask you a series of questions which will help formulate a hypothesis as to why you have your pain. Questions such as why your pain started, how long you have had your pain, what aggravates your symptoms and what eases your symptoms will be asked. A full medical history will also be documented. This is to uncover any possible medical conditions that could be causing your pain such as systemic inflammation arising from rheumatoid arthritis.
- Physical assessment – your clinician will assess your knee using a series of tests including joint range of movement, muscle flexibility and strength, and palpation of different structures surrounding the knee. Your clinician will also ask you to perform a set of simple functional tasks often including single-leg balance and single-leg squatting, lunging and jumping. They may also analyse your walking and running style.
The clinical assessment is normally sufficient to diagnose a patella tendinopathy. However, a clinical assessment is limited in providing any further information about the tendon structure and surrounding tissues. This is very important especially if your symptoms are not improving.
Diagnostic musculoskeletal ultrasound imaging
A diagnostic ultrasound scan is carried out on your first session to gain more information. A scan will be able to answer the following questions:
- How severe is the tendinopathy?
- Is there a tear in the tendon?
- Is there inflammation of the surrounding bursa?
- Is there inflammation of the fat pad?
- Is there involvement of other structures such as the meniscus (cartilage in the knee)
Diagnostic ultrasound scan is able to assess tendon structure and inflammation associated with tendinopathy. Ultrasound is regarded as the gold standard imaging technique for assessing tendon structure and pathology (Dan et al., 2018). It shows the internal structure of the tendon better than on an MRI scan.
Complete Injections clinicians are all highly experienced physiotherapists and musculoskeletal sonographers. During your initial assessment, you will be provided with a formal diagnosis using a combination of clinical examination and diagnostic imaging after which the clinician will be able to prescribe the most appropriate treatment for your condition.
How do we treat patella tendinopathy in the knee?
Patella tendinopathy is notoriously challenging to rehabilitate and therefore it is essential that treatment starts as early as possible (Cong et al., 2016). Rehabilitation of jumper’s knee requires specialist physiotherapy intervention involving any number of the following techniques:
- Advice on activity modification allowing the patellar tendon to rest and heal appropriately.
- Hip and knee strengthening exercises. Research has shown that heavy slow resistance (HSR) exercises can have a positive effect on patellar tendinopathy (Kongsgaard et al, 2009).
- Biomechanical re-education – this may involve teaching you how to correctly squat, run or jump.
- In some cases, your clinician may perform soft tissue manipulation techniques or acupuncture to help reduce any pain that might be making your rehabilitation exercises difficult to perform.
- Advice on taping or using a patellar tendon support during sport.
Research shows that a rehabilitation programme for patella tendinopathy should be carried out for 3 months before considering further intervention such as injections or shockwave therapy.
What if physiotherapy does not work?
Physiotherapy will always be the pillar of your treatment, but there are other options alongside physiotherapy to assist your progress along if required:
Extracorporeal shockwave therapy (ESWT)
Shockwave therapy produces a series of powerful sound waves which provide a small dose of controlled microtrauma to the patella tendon. Research has shown that shockwave stimulates the tendons natural healing process, initiating a new healing process. Local nerve endings surrounding the painful tendon become desensitised by these pulses, resulting in pain and symptom reduction.
Recent evidence suggests positive outcomes following 3-5 shockwave treatment sessions running concurrently with a progressive loading exercise program for the treatment of all lower limb tendinopathies (Zwerver et al, 2010). All clinicians at Complete are trained to deliver shockwave. If you would like more information regarding shockwave therapy please contact us on 0207 4823875 or email injections@complete-physio.co.uk.
Injection therapy
If your pain has persisted for over 3 months and you have not improved with physiotherapy then you may be appropriate for injection therapy. Injection therapy has historically been used within musculoskeletal medicine to reduce pain and inflammation allowing you to effectively rehabilitate your condition.
It is of particular value in the following circumstances:
- Your pain is affecting your ability to sleep or is waking you during the night.
- Your pain is significantly limiting your ability to perform normal activities of daily living or partake in sports or leisure activities.
- Your pain is affecting your ability to undertake your rehabilitation exercises.
- Your pain is getting worse or your progress has plateaued.
- You have embarked on a 3-month rehabilitation programme with little or no improvement
There are two injection options for patella tendinopathy.
1. Ultrasound-guided high-volume injection
When the patellar tendon becomes tendinopathic, the internal structure of the tendon becomes compromised. Tendinopathic change drives a process called neovascularisation. Neovascularisation is the growth of new blood vessels within and around the tendon. These new vessels are accompanied by very small nerves. It is hypothesised that these small nerves are responsible for some of the pain associated with patella tendinopathy.
An ultrasound-guided high-volume injection uses a combination of saline (sterile water) and a local anaesthetic to obliterate these small vessels and nerves and reduce pain. This technique has been practised for over 10 years and has some evidence to support its use (Barker-Davies et al, 2017). On occasion, a small dose of corticosteroid (also known as steroid) may be added to the injection. Steroid is a potent anti-inflammatory and is reserved for very irritable and inflamed cases.
Current research has raised concerns surrounding steroid injection for treating patellar tendinopathy. This is due to a small increased risk of tendon rupture following the procedure and therefore, corticosteroid injection should be used judiciously (Resteghini et al., 2016). The use of steroid in your specific case will be discussed following your assessment and ultrasound scan.
2. Ultrasound-guided platelet-rich plasma (PRP) injection
PRP has been clinically proven to enrich the healing process and speed recovery of tendons. It has been shown to be a safe treatment for patellar tendinopathy. Although there is evidence to support its use in patella tendinopathy, the evidence to supports its use is minimal and there is conflicting evidence. It is reserved for cases that have failed to respond to all other treatment options (Cong et al., 2016).
PRP requires a small amount of blood to be extracted from a vein in your arm. Blood is then spun, at high speeds, in a centrifuge machine. This separates the PRP from other blood molecules. PRP is then injected, under guidance, in and around the patellar tendon. Research has suggested a series of three injections is required to successfully treat tendinopathic pain.
Using ultrasound guidance is essential to ensure the accuracy of the injection and limit any potential side effect. Ultrasound-guided injections are better tolerated by patients with less procedural pain. At Complete, to ensure you experience the maximum benefit with the least discomfort, all injection techniques are performed using ultrasound guidance.
Complete Injections offers a same day service on all guided injections. All clinicians are independent prescribers, musculoskeletal sonographers and injection therapists. You are able to self-refer directly into our service, you do not need to be referred by your G.P. If you would like more information or would like to book an appointment please contact us on 0207 4823875 or email injections@complete-physio.co.uk.
Related conditions, blogs and patient’s stories from our specialists
Our highly experienced team of expert clinicians have written a selection of blogs on various treatment methods for Jumper’s knee, some stories from patients that came to us seeking relief from their knee pain, as well as explanations of other knee conditions that might be causing your pain. Please take a look at any of the following links and get in touch with us if you think you are suffering from any of these conditions and may require treatment.


Leave A Comment