What is patellofemoral joint (PFJ) pain (pain behind the knee cap)?
Patellofemoral joint (PFJ) pain cause pain at the front of the knee. The pain is often hard to pinpoint and feels deep in the joint or ‘behind the knee cap’. It is more common in females then males and is often aggravated by prolonged walking particularly downstairs and/or down hill’s, squatting, lunging and running. It can be worse after sitting still for a while and the pain is often associated with clicking. Patellofemoral joint pain can cause intermittent swelling but not always.
The initial diagnosis can be made by clinical assessment alone, and no formal imaging is required. However, if your pain is not improving imaging can help to confirm the diagnosis and assess for any structural changes especially to the cartilage on the back of knee cap. Imaging can also the assess the contribution of surrounding structures such as patella tendinopathy (Jumper’s knee), ITB friction syndrome (Runner’s knee), pes anseurine bursitis and fat pad inflammation.
There is no quick fix for patellofemoral joint pain. Most patellofemoral joint pain resolves with a comprehensive course of physiotherapy. Physiotherapy may involve hands on treatment, taping techniques to reduce your pain and a progressive loading programme to improve the strength and mechanics of your leg.
Ultrasound guided steroid injections do have a role to play in the treatment of some patellofemoral joint pain. A steroid injection may be indicated if:
- your pain is not improving
- you are waking you up at night
- if you are not improving despite a comprehensive course of physiotherapy
- you cannot engage in a course of physiotherapy due to high levels of pain
Injections should always be followed up with a course of physiotherapy. Hyaluronic acid, are a drug-free alternative to steroid injections and can also provide pain relief.
What are the symptoms of patellofemoral joint (PFJ) pain?
The symptoms of osteoarthritis of the knee are:
- Pain on the front of the knee, which often comes on for no obvious reason
- Pain is aggravated by walking downhill particularly but also squatting, lunging and running
- Pain that does not respond to rest
If this sounds like your pain, read on below…
What other conditions can mimic patellofemoral joint (PFJ) pain?
If this does not sound like your pain there are other conditions that can mimic the pain of osteoarthritis knee, such as:
- Fat pad inflammation
- Cartilage (meniscal) tear
- Patella tendinopathy (Jumper’s knee)
- ITB friction syndrome (Runner’s knee)
- Pes anseurine bursitis
Patellofemoral joint pain versus patella tendinopathy
Patellofemoral joint pain causes pain on the front of the knee that is hard to pinpoint i.e., it can be difficult to find a specific tender spot, whereas patella tendinopathy pain is very specific and easy to locate. If you have patella tendinopathy, simply pressing the tendon on the front of the knee will reproduce your symptoms. It is unlikely to be patella tendon tendinopathy if you do not have this specific tenderness.
Furthermore, patella tendinopathy pain normally improves with exercise and is worse after exercise, often lasting for a few days. Whereas patellofemoral knee joint pain normally does not improve with exercise and often increases as you continue exercises.
The anatomy of the knee
The patellofemoral joint (PFJ) is one of the two joints which make up the knee complex. The patella (kneecap bone) is located at the front of the knee and is responsible for increasing the strength and power of the quadriceps (the large muscle group at the front of the thigh).
The patellofemoral joint is created by the patella (kneecap bone) and the femoral condyles of the femur (two large bony prominences located at the end of the long bone of the upper thigh). These two bony prominences create a central concave ‘V’ shaped groove (known as the trochlea) which perfectly fits the back of the patella, which has a reciprocally convex shape.
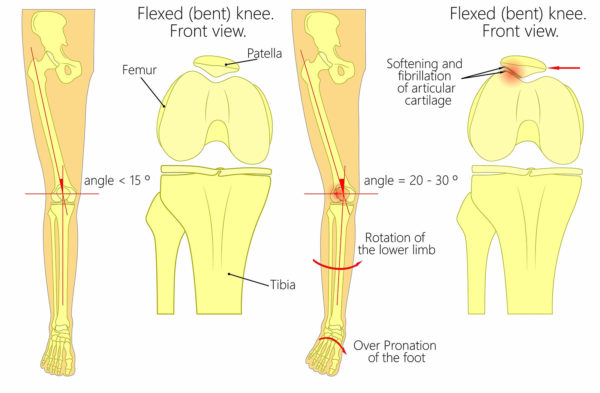
The trochlea and the back of the patella are both covered in a layer of articular cartilage. Articular cartilage provides a smooth, low friction surface for the bones to glide over one another during movement. Evidence has demonstrated that articular cartilage requires movement of the joint to maintain a healthy structure. However, research has also shown that abnormal loading of the joint causes the articular cartilage to negatively alter its composition. This negatively altered composition weakens its structure, causing the articular cartilage to become thinner (Clarke et al., 2003). If this continues it can progress to what is known as osteoarthritis. Further research has suggested that maintaining good flexibility and strength around the joint will help to slow the disease progression associated with osteoarthritis (Hunter et al., 2009).
Osteoarthritis is the most common musculoskeletal pathology effecting up to 15% of the world’s population (Hubbert et al., 2018). It causes pain and disability and is especially debilitating when affecting weight-bearing joints such as the hip, knee or ankle. The hip and knee are the two most commonly affected joints. Current evidence suggests that PFJ osteoarthritis is responsible for 8% of all cases of osteoarthritis (Kanazawa et al., 2017) and is caused by a multitude of factors.
Risk factors associated with patellofemoral osteoarthritis include:
- Sex – recent studies have shown a slightly increased rate of patellofemoral osteoarthritis in women (13.6 to 24%) compared with men (11 to 15.4%) (Kanazawa et al., 2017)
- Age – patellofemoral osteoarthritis is most commonly observed from the fifth decade onwards (Kanazawa et al., 2017)
- Hip muscle weakness – strength deficits in the hip can adversely affect lower limb alignment and have been shown to significantly increase the risk of patellofemoral osteoarthritis (Souza et al., 2009)
- Femoral structure – the upper end of the femur (the long bone of the thigh) forms the ball of the hip joint. In some people the angle of this ball-shaped end of the femur is altered. This is called femoral anteversion and has been linked with increased risk of patellofemoral osteoarthritis (Souza et al., 2009)
- Patella position and structure – if the back of the patella does not align within the trochlea of the femoral condyles precisely, adverse pressure is piled on the articular cartilage resulting in osteoarthritic change
- Weight – high body mass index (BMI) has been linked to the onset of osteoarthritis
- Repetitive overloading of the patellofemoral during certain types of activity such as running, jumping and hopping
- Poor foot biomechanics – excessive pronation (flat foot) can result in increased pressure through the PFJ
How do you know if you have patellofemoral osteoarthritis?
Patellofemoral osteoarthritis is a progressive, degenerative disease which can take many months or even years to develop prior to symptoms being felt.
Common symptoms or features associated with patellofemoral osteoarthritis include:
- Pain located at the front of the knee, often aggravated during walking and stair climbing
- Audible clicking of the patella during movement, such as squatting or kneeling
- Swelling and ‘puffiness’ located around the patella
- Pain and stiffness after periods of inactivity – patellofemoral pain is often worse first thing in the morning or after sitting for prolonged periods of time
- Poor balance, especially when standing on one leg – lower limb strength is important for maintaining good balance. As previously mentioned, hip weakness has been associated with the onset of patellofemoral osteoarthritis
How is patellofemoral osteoarthritis diagnosed?
It is essential that an accurate diagnosis of patellofemoral osteoarthritis is obtained. Diagnosis of this condition includes clinical examination and the use of diagnostic imaging.
Clinical examination
The clinical examination enables the clinician to clarify the hypothesis of patellofemoral osteoarthritis and formulate an appropriate treatment plan. Physiotherapy is a key treatment modality for patellofemoral osteoarthritis.
The clinical examination reveals factors involved in the development of your pain and includes the following steps:
- An in-depth interview is used to reveal how, what, why and when your pain started. You will also be asked questions such as what aggravates and eases your symptoms. A full medical history will also be taken to rule out systemic causes of your pain such as rheumatoid arthritis. If your clinician suspects a systemic cause of your pain, you may be referred for further investigations.
- The physical examination includes testing knee joint range of movement, assessing strength and flexibility of the surrounding muscles, palpation (feeling) of the knee structures and functional testing such as squatting, single leg balance, gait analysis, and running analysis (if you are runner).
Although the clinical examination can provide a wealth of information, it is unable to definitively diagnose PFJ osteoarthritis. For this, diagnostic imaging is required.
X-ray

If your clinician suspects the presence of osteoarthritis you may be referred for an x-ray. X-ray is regarded as a gold standard imaging technique capable of accurately diagnosing the presence and severity of bone and joint pathology, including osteoarthritis (see above image).
Diagnostic musculoskeletal ultrasound imaging
Diagnostic musculoskeletal ultrasound imaging has been shown to be a highly effective imaging tool for visualising factors associated with osteoarthritis. It is capable of detecting early-stage osteoarthritic changes within the bony contours of the patella and the trochlear groove. Ultrasound is also excellent at visualising swelling (known as an ‘effusion’) and inflammation of the joint (known as ‘synovitis’) (Kaeley et al., 2020, Wakefield et al., 2000).
Clinicians at Complete are highly experienced and are dual qualified in both physiotherapy and musculoskeletal sonography. During your initial assessment a comprehensive clinical assessment and diagnostic musculoskeletal ultrasound scan will be performed.
How do we treat patellofemoral osteoarthritis?

The vast majority of patients are able to effectively manage the pain and symptoms of patellofemoral joint pain using conservative measures. Maintaining good flexibility and strength around the affected joint are the two most important factors associated with the management of osteoarthritis (Hunter et al., 2009). Physiotherapy should form the foundation of your treatment.
Physiotherapy treatment for patellofemoral joint pain regularly includes:
- Hip and knee muscle strengthening exercises
- Hip and knee stretching techniques
- Biomechanical re-education – this may involve re-education of certain movement patterns
- Advice on activity modification and relative rest
- Advice on using ice and taping to manage symptoms
- Occasionally your clinician may use joint manipulation, acupuncture or soft tissue techniques to help you manage your pain and symptoms. This will allow you to partake in your exercise programme more effectively.

Here are a few tips and tricks you may wish to try:
- Avoid aggravating your knee pain – this may mean modifying activities of daily living or resting from tasks or hobbies that irritate your knee, such as jogging
- Strength training – strengthening your knee musculature is the foundation of conservative treatment
- A knee brace with a hole at the front may be a useful adjunct to control pain (these do not help everyone – see image below)
- Use an ice pack or a small bag of peas wrapped in a damp towel, placing it over your knee to help reduce pain and inflammation
- Try using an anti-inflammatory gel such as Voltarol to help manage your symptoms. Please speak to your pharmacist before starting any medication.

What if conservative management does not work?
If a course of physiotherapy and a progressive home exercise program has not sufficiently helped you, then injection therapy may be appropriate.
Injection therapy is used to reduce pain and inflammation associated with osteoarthritis and can provide you with a ‘window of opportunity’ to effectively rehabilitate your knee in a pain-free environment.
Injection therapy is particularly helpful if you are suffering one or more of the below scenarios:
- Pain is affecting your ability to sleep or is waking you up at night
- Pain is limiting your activities of daily living
- Pain is affecting your ability to work or partake in leisure activities
- Pain is limiting your ability to complete your physiotherapy programme
All injections at Complete are carried out using ultrasound guidance. Ultrasound guided injections have shown high levels of accuracy, reduced post injection complications and increased levels of pain relief when an injection is performed under ultrasound guidance.
At Complete Injections our highly trained team of clinicians are qualified to performing ultrasound-guided injections for patellofemoral knee joint pain. All clinicians are experienced physiotherapists, musculoskeletal sonographers, independent prescribers and injection therapists who are able to perform a same day injection service on all guided injections. You can self-refer directly into our service. You do not need to see a GP first.
There are two ultrasound-guided injection options available for the treatment of patellofemoral osteoarthritis:
Ultrasound-guided corticosteroid injection
During a steroid injection an ultrasound machine is used to accurately place the needle to deposit a combination of corticosteroid (powerful anti-inflammatory medication) and short-acting local anaesthetic directly to the point of your pain. Corticosteroid injection is an effective treatment for reducing pain and inflammation associated with osteoarthritis.
Ultrasound-guided hyaluronic acid injection
The Hyaluronic acid injection technique uses a natural (non-drug) synthetic version of the joint’s natural lubricant. Hyaluronic acid has also been shown to have powerful anti-inflammatory properties and is regularly used as an alternative to the corticosteroid for the treatment of osteoarthritis.
Injection therapy should not be used as a stand-alone treatment. For the best, long-term results it is important that you use the pain relieving effects of the injection to commence a programme of physiotherapy within 2 weeks.
If you would like more information or would like to book an appointment, please contact us on 0207 4823875 or email injections@complete-physio.co.uk.
Related conditions, blogs and patient’s stories from our specialists
Our highly experienced team of expert clinicians have written a selection of blogs on various treatment methods for knee pain, some stories from patients that came to us seeking relief from their knee pain, as well as explanations of other knee conditions that might be causing your pain. Please take a look at any of the following links and get in touch with us if you think you are suffering from any of these conditions and may require treatment.


Leave A Comment