Anatomy of the foot
The foot is designed to provide strength, balance, stability, and flexibility. This is achieved by a complex series of 33 joints (26 bones) all of which articulate together to perform a complex array of movements.
The foot is divided into three main areas (as seen in below image):
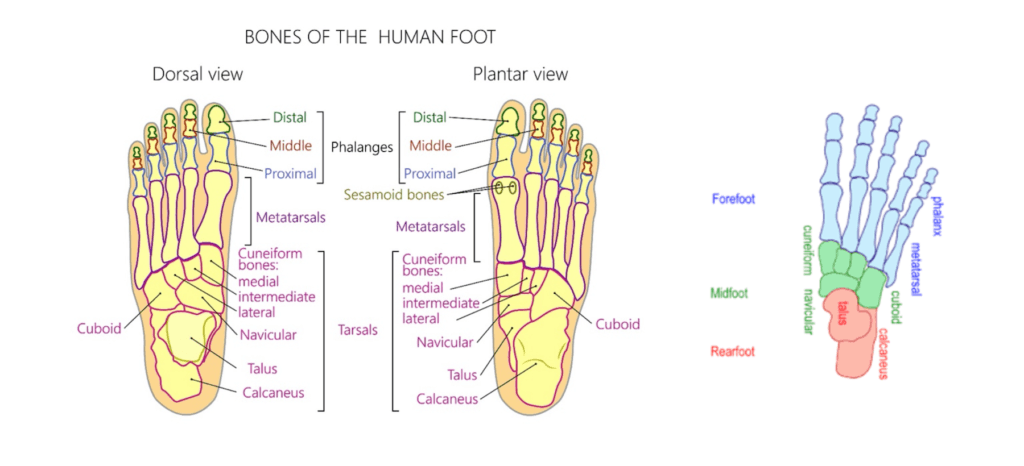
The rear foot and ankle.
The rear foot and ankle consist of four bones:
- The tibia (large long bone of the shin)
- The fibula (smaller long bones of the session)
- The talus (ankle bone)
- The calcaneus (heel bone)
These 4 bones create two joints.
The talocrural joint is created by the articulation of the talus bone with the tibia and fibula bones of the shin and is responsible for dorsiflexion (flexing the ankle such as when stretching of calf) and plantarflexion (pointing your toes down such as when wearing high heels).
The talus and the calcaneus bones articulate to create the subtalar joint which is responsible for Inversion and eversion (turning your ankle inwards and outwards respectively).
The midfoot (section of foot further discussed within this blog)
The midfoot is created by the articulation of five irregular shaped bones. These bones are:
- The cuboid
- The navicular
- The lateral cuneiform
- The middle cuneiform
- The medial cuneiform
The midfoot provides:
- A flexible, shock absorbing arch which allows you to finetune your interaction with the ground
- Delivers a rigid lever for ambulation (Thomas et al., 2015. Chi et al., 2000)
The forefoot
The forefoot consists of the long bones that creates the five digits or toes of the foot.
The long bones of the forefoot are called:
- The metatarsals
- Phalanges
Due to the multifaceted demands placed on the midfoot during weight-bearing and locomotion this area of the foot is often associated with developing osteoarthritis.
The articulating surfaces of the five bones of the midfoot create a complex web of joints. These joints are covered in a protective, friction reducing coating called articular cartilage. When a joint is subjected to repetitive or inappropriate loading the articular cartilage can become thinner, putting more pressure on the underlying bone. This progressive process is called osteoarthritis. When osteoarthritis is present a thin layer of connective tissue within the joint capsule, called the synovium, also becomes irritated. The resulting synovial inflammation is called synovitis and has been linked with the progression of osteoarthritis and is often responsible for the episodic painful flare ups in symptoms associated with osteoarthritis.
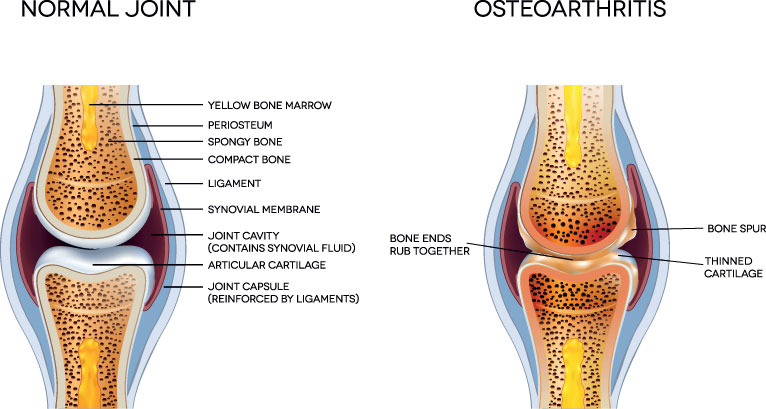
Osteoarthritis commonly affects weight-bearing joints and is often observed in the hip and ankle.
There are many risk factors involved in developing osteoarthritis (Thomas et al., 2015):
- Age – the prevalence of osteoarthritis increases with age. Midfoot osteoarthritis has been observed in 12% of the population over the age of 50, with most symptomatic cases observed in patients over 75.
- Sex – females have been shown to be more susceptible to developing midfoot osteoarthritis than males.
- Increasing body weight – as bodyweight increases so does the pressure on your load-bearing joints. This extra weight on the small joints of the mid foot can cause increased pain associated with osteoarthritis.
- Trauma – previous fractures can disrupt the joint surfaces resulting in articular cartilage damage
- Poor biomechanics and muscle weakness – if your body weight is not evenly dispersed over the foot, due to weak calf and hip muscles, poor lower limb alignment, leg length discrepancy, poorly fitting shoes, or an altered walking and/or running style then pressure on the midfoot joints can increase and cause more pain.
- Sporting activities or your occupation – can put excessive pressure on your midfoot joints, over many years resulting in arthritic changes for example football or running.
- Diabetes – this is probably related to compromised blood flow to the foot but the exact mechanism is not known.
How do you know if you have midfoot osteoarthritis?
Midfoot osteoarthritis is a progressive, degenerative condition which typically takes many months or even years to develop before becoming symptomatic.
|
Symptoms of midfoot osteoarthritis include:
|
How is midfoot osteoarthritis diagnosed?

Obtaining an accurate diagnosis of midfoot osteoarthritis is essential and informs that clinician of the most appropriate treatment options available for you. Midfoot osteoarthritis is diagnosed using a combination of clinical assessment and diagnostic imaging. An X-ray (see image above) or an MRI scan are the gold standard for the diagnosis of osteoarthritis of the foot.
Clinical assessment
The clinical assessment is used to help formulate a hypothesis of osteoarthritis. A formal diagnosis of osteoarthritis cannot be created with clinical assessment alone. However, clinical assessment is able to uncover the factors associated with your pain, it is essential for corrective rehabilitation and is an important part of diagnosis process.
Assessment of midfoot osteoarthritis is typically conducted by an orthopaedic consultant, podiatrist or a physiotherapist and involves the following:
Physical assessment
Physical assessment includes:
- Structural assessment of your foot including reviewing the arch of your foot
- Foot and ankle joint range of motion on assessment
- Calf and foot muscle strength testing
- Palpation (feeling) joints of the foot
- Functional testing including assessment of your gait
- Assessment of footwear
On completion of the clinical assessment your clinician may request further diagnostic tests. These may include:
Blood tests
If your symptoms are thought to be due to a systemic inflammatory disorder then you may be referred for a series of blood tests. This can be carried out by your GP or a specialist.
X-ray (above image) or MRI scan
If your clinician believes you have midfoot osteoarthritis, you maybe referred for an X-ray or an MRI scan. Both are considered the gold standard imaging tool for assessing bone and joint pathology, including fractures and osteoarthritis. A formal diagnosis of osteoarthritis can be hypothesised but not confirmed without X-ray or an MRI. Both are able to visualise the presence of osteoarthritis and the severity of the process. However, many people exhibit symptoms which do not correlate with X-ray findings. If synovitis is present, within the affected joint, symptoms may be significantly worse than expected. Synovitis is best visualised on diagnostic ultrasound (more later) Conversely many patients exhibiting severe osteoarthritis on imaging are able to function very well with minimal symptoms.
Diagnostic musculoskeletal ultrasound imaging
Diagnostic musculoskeletal ultrasound has been proven to be a highly effective imaging technique for assessing the swelling and inflammation associated with synovitis. It has also been shown to be able to pick up early bony changes on joints such as bony osteophytes and corticol irregularity, associated with osteoarthritis (Wakefiled et al, 2000. Kaeley et al, 2020).
Complete has a team of highly experienced practitioners holding dual qualifications within physiotherapy and musculoskeletal sonography. During your initial assessment your clinician will conduct a full clinical assessment and diagnostic scan. If you would like more information or would like to book an appointment please contact us on 0207 4823875 or email injections@complete-physio.co.uk.
How do we treat midfoot osteoarthritis?

Midfoot osteoarthritis is often overlooked, with many people suffering from their symptoms for many years before seeking professional help. To experience maximum benefit from treatment it is important that treatment starts as early as possible.
Many people respond positively to physiotherapy rehabilitation for the management of midfoot osteoarthritis. Research has shown that maintaining good levels of flexibility and strength around the affected joints are essential in maintaining function and managing the symptoms associated with osteoarthritis.
Physiotherapy treatment regularly includes:
- Advise on activity modification and pain management
- Calf stretching exercises
- Hip, calf and foot muscle strengthening exercises are often prescribed to correct muscle imbalances within the lower limb which may be contributing to midfoot osteoarthritis
- Joint manipulation and soft tissue techniques to the joints and surrounding muscles of the foot and ankle, this helps reduce your pain and improve function
- Orthotics (insoles) or physio taping techniques may be used to off load the midfoot joints. Occasionally an onward referral to a podiatrist is required for customised orthotics (Dugarte et al., 2016) (see below image)

Here are some tips and tricks you may like to try yourself:
- Rest from aggravating activities. If this is not possible try to modify these as best you can. This may include taking regular breaks or using a stick to help you walk.
- Losing weight will reduce pressure through your foot resulting in a reduction in pain and symptoms.
- Try some gentle calf stretches.
- Calf strengthening exercises such as heel raises can help strengthen your ankle muscles. Always start double leg and then progress to single leg if pain allows.
- Over-the-counter oral medication such as paracetamol or ibuprofen or a topical anti-inflammatory gel such as Voltarol can be effective at reducing pain associated with osteoarthritis. Talk to your pharmacist before taking medication.
What if conservative management does not help?
If your symptoms remain persistent and you have undertaken a course of physiotherapy and rehabilitation exercises then an injection may be beneficial for you.
Ultrasound guided injection therapy has been used for many decades to treat the pain and inflammation associated with osteoarthritis and is particularly effective in the following situations:
- Symptoms that persist for over 3 months
- Symptoms that affect your sleep
- Symptoms that limit your ability to complete activities of daily living
- Symptoms that limit your ability to work or partake in leisure activities
- Symptoms that affect your ability to complete a physiotherapy rehabilitation program
An injection is not a standalone treatment. Research has shown for maximum benefit to be achieved an injection should be used in conjunction with physiotherapy. At Complete we recommend a course of treatment commence within two weeks after your injection for midfoot osteoarthritis.
Current evidence has revealed that musculoskeletal injections completed under ultrasound guidance are better tolerated by patients, more accurate and have less post injection complications than landmarks injections. This technique uses diagnostic ultrasound to create real-time imaging of target tissue, allowing for visualisation of the needle tip and accurate deposition of the medication directly to the centre of your pain. The space between the bones of the mid-foot joints is only a few millimetres and so all foot injections at Complete are carried out under ultrasound guidance for maximal effect.
There are two ultrasound-guided injection options available for the treatment of midfoot osteoarthritis:
1. Ultrasound-guided corticosteroid injection
A corticosteroid is a strong, injectable anti-inflammatory medication that has been used for decades to effectively reduce pain and inflammation associated with osteoarthritis. Corticosteroid is combined with a local short acting analgesic prior to being injected under ultrasound imaging. The combination of ultrasound imaging and short-acting local analgesic allows for an accurate comfortable injection experience.
2. Ultrasound-guided hyaluronic acid injection
Hyaluronic acid is a man-made replica of a naturally occurring substance found within joints. It provides lubrication for the joint and has been shown to possess powerful anti-inflammatory properties. It is regularly used, in combination with short-acting local anaesthetic, as an alternative to the corticosteroid for the treatment of osteoarthritis.
Complete are able to provide you with a same day service on all injections. You do not need a referral from your G.P. You are able to self-refer directly into our service. Our highly experienced team of clinicians are fully qualified independent prescribers, physiotherapists, musculoskeletal sonographers and injection therapists who will be able to assess, diagnose, prescribe the most appropriate medication and complete an injection all within the same session.
If you would like more information or would like to book an appointment please contact us on 0207 4823875 or email injections@complete-physio.co.uk.
Other foot and ankle conditions:
References
Dugarte, A., Bharwani, S., Yoo, H., Boiwka, A.V., Charles, C.Y., Bajwa, N.S., Toy, J.O., Tang, J.E., Ahn, U. and Ahn, N., 2016. Calcaneocuboid joint arthritis of the midfoot precedes tibiotalar joint arthritis. Orthopedics, 39(6), pp.e1112-e1116.
Chi, T., Tencer, A. and Sangeorzan, B., 2000. The role of foot structures in control of midfoot motion. In 46th annual meeting of the Orthopedic Research Society.
Kaeley, G.S., Bakewell, C. and Deodhar, A., 2020. The importance of ultrasound in identifying and differentiating patients with early inflammatory arthritis: a narrative review. Arthritis Research & Therapy, 22(1), pp.1-10.
Thomas, M.J., Peat, G., Rathod, T., Marshall, M., Moore, A., Menz, H.B. and Roddy, E., 2015. The epidemiology of symptomatic midfoot osteoarthritis in community-dwelling older adults: cross-sectional findings from the Clinical Assessment Study of the Foot. Arthritis research & therapy, 17(1), p.178.
Wakefield, R.J., Gibbon, W.W., Conaghan, P.G., O’Connor, P., McGonagle, D., Pease, C., Green, M.J., Veale, D.J., Isaacs, J.D. and Emery, P., 2000. The value of sonography in the detection of bone erosions in patients with rheumatoid arthritis: a comparison with conventional radiography. Arthritis & Rheumatism, 43(12), pp.2762-2770.


Leave A Comment