What is a chronic ankle ligament sprain (also known as chronic ankle instability)?
The outer (lateral) aspect of the ankle is stabilised by a series of ligaments. These ligaments are commonly sprained when tripping over, twisting the ankle or during a tackle whilst playing football. When these ligaments are injured, the ankle can become unstable resulting in further ligament sprains and continued pain. Nearly half of all patients who sustain an ankle ligament sprain report long term ankle pain and instability.
What are the symptoms of a chronic ankle ligament sprain?
Symptoms of a chronic ankle ligament sprain are:
- A history of a significant traumatic event
- Multiple ankle injuries over time
- Swelling and bruising over the outer aspect of the foot and ankle after injury
- Cracking noises from the ankle with walking
- Ankle stiffness
- Pain around the lateral malleolus (the large bony bump on the outside of the ankle)
What other conditions can present like a chronic ankle ligament sprain?
Other conditions which can present as a chronic ankle ligament sprain include:
Chronic ankle ligament sprain vs ankle joint osteoarthritis
The site of symptoms can also help to differentiate between these conditions. A chronic ankle ligament sprain is primarily felt over the outside of the ankle, in comparison to ankle osteoarthritis (OA) which is more widely spread and felt across the top of the foot as well as on the outer and inner aspects of the ankle.
Ankle osteoarthritis (OA) is a common complaint in the older population and affects both men and women alike, it can occur after trauma but more commonly develops slowly over a long period of time. The pain associated with ankle osteoarthritis is often linked with a progressive stiffness and a change in shape of the ankle joint. A chronic ankle ligament sprain is more commonly associated with trauma i.e. a ‘twisted ankle’. It also affects men as much as women but is much more common in a younger sporting/active population.
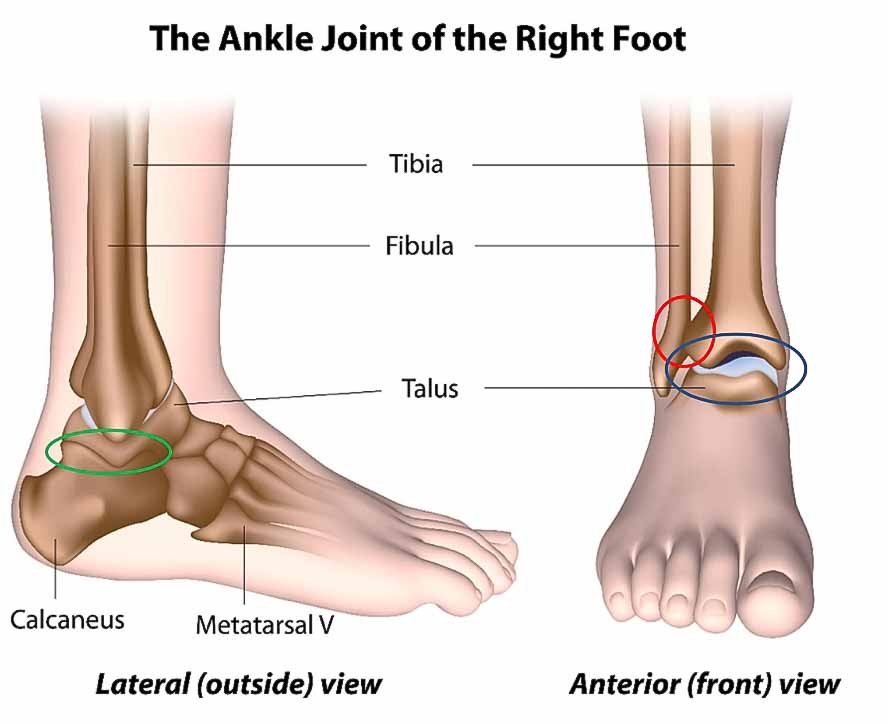
Anatomy of the ankle
The ankle is a complex region consisting of three separate joints which are responsible for producing the following actions (see image below):
- The talocrural joint (the ankle joint proper – blue arrow below) is created by the tibia, fibula and talus bones. It is responsible for dorsiflexion (pulling your foot towards the sky) and plantarflexion (pointing your foot towards the ground).
- The inferior tibiofibular joint (red circle below) is created by the tibia and the fibula bones and is responsible for stabilising the lower shin and the ankle.
- The subtalar joint (green circle below) is formed by the talus and the calcaneus bones and is responsible for inversion (turning your ankle in) and eversion (turning your ankle out).
Ligaments
Ligaments are short, strong fibrous bands of tissue that connect bones together, forming joints. A ligament is designed to provide mechanical reinforcement to the joint, increasing its strength and stability (Singh et al., 2016). They are structurally rigid and designed to resist and control excessive movement from occurring at the joint (Hauser et al., 2011). Ligaments are also rich in proprioceptive cells (cells used to provide sense of awareness of body position, increasing balance and stability). When a ligament is injured balance and joint stability is negatively affected. A reduction in balance and stability causes an abnormal transition of force through the joint surface, increasing the risk of osteoarthritis (Hauser et al., 2011).
Ankle ligaments
The ligaments of the ankle are divided into 3 groups. The lateral ligaments (ligaments on the outside of the ankle), these will be at the centre of discussion within this blog. The medial ligaments (ligaments located on the inside of the ankle) and the high ankle ligaments (ligaments stabilising the tibia and fibula of the shin).
The lateral ligaments
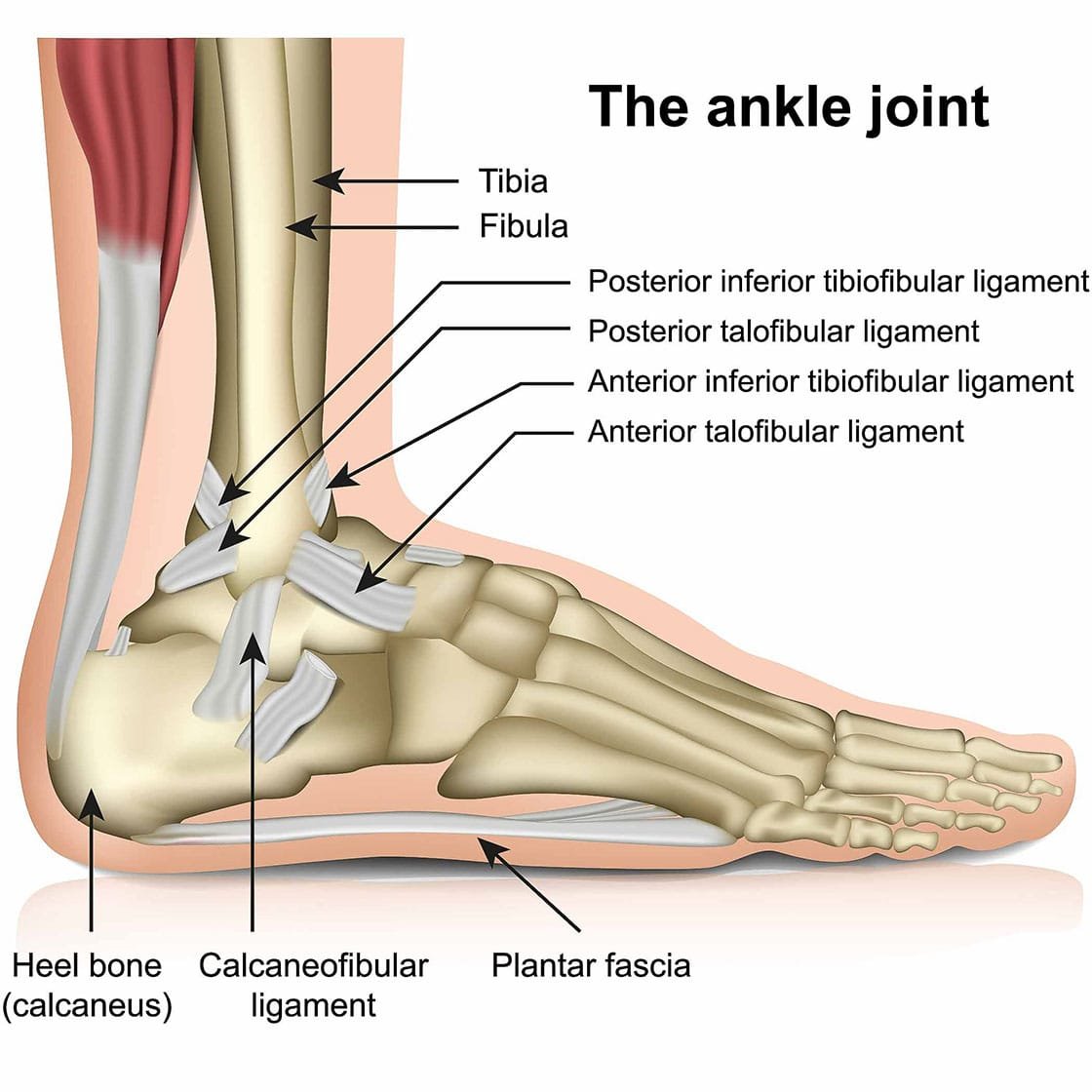
There are 3 lateral ankle ligaments, these are as follows:
- The anterior talofibular ligament (ATFL). This ligament attaches the lateral malleolus of the fibular (large bony prominence at the end of the fibula) to the talus bone of the ankle.
- The calcaneofibular ligament (CFL). This ligament attaches the calcaneous (heel bone) to the tip of the lateral malleolus of the fibula.
- The posterior talofibular ligament (PTFL). This ligament attaches the posterior aspect (rear) of the talus to the lateral malleolus of the fibula.
Lateral ankle ligament injuries are surprisingly common. A large national survey observed 630,890 ankle injury sprains occurred in England in 2009 alone (Woodman et al., 2013).
Lateral ankle ligament sprains occur when the ankle is subjected to an unexpected, high velocity trauma involving inversion and plantarflexion (see below image). A lateral ankle injury resulting in a ‘twisted ankle’ commonly occurs:
- Tripping off a curb.
- Whilst playing football, often during a bad tackle.
- Stumbling in high heels.
- Running on Cobblestones.

Common symptoms associated with lateral ankle injury includes:
- Sudden traumatic event involving twisting or rolling your ankle.
- Popping or cracking sound emanating from your ankle may be heard.
- Immediate swelling. This can be significant with severe sprains and often develops overnight resulting in a large egg-shaped swelling over the lateral ankle.
- Bruising. In cases of significant lateral ankle ligament injury bruising can cover the whole ankle and track into the foot (see below image)
- Stiffness. Stiffness is often associated with inflammation and is particularly worse after prolonged periods of rest such as sitting at your desk or waking in the morning. Stiffness often is relieved with movement.
- Pain located over the ATFL ligament located just in front of the lateral malleolus

Lateral ankle ligament injury stats:
- Out of the three lateral ligaments of the ankle, the ATFL is the weakest and most prone to injury (Singh et al., 2016. Li et al., 2017).
- 70% recurrence rates have been observed following lateral ligament injury of the ankle (Hubbard and Hertle et al., 2006).
- 10% of patients with lateral ankle sprains fail conservative management (Lee et al., 2017).
- 40% of patients suffering lateral ankle ligament injury report persistent chronic (pain persisting for over 12 weeks) pain interfering with activities of daily living (Golano et al., 2016).
- 20% of patients suffering from chronic lateral ankle have been observed to have not only sprain ATFL but also the CFL (Golano et al., 2016).
How do we diagnose a lateral ankle ligament sprain?

Lateral ankle ligament sprains are routinely diagnosed using a clinical assessment and diagnostic imaging. The clinical assessment should be carried out by a highly experienced physiotherapist and includes an interview and a physical assessment. The interview is designed to reveal how your pain started, whether this is the first time you have experienced an ankle injury, any previous trauma or pathology in the leg (from the hip to the big toe) and what aggravates or eases your symptoms.
The physical assessment comprises of:
- Close inspection of the foot and ankle assessing for swelling and bruising.
- Structural assessment of your ankle and foot (including assessing the quality of the arch of your foot).
- Foot and ankle joint range of motion. Inversion and eversion are of particular importance when assessing lateral ankle ligament sprains.
- Calf muscle strength testing. Can you complete a heel raise?
- Balance testing. Can you stand on one leg and maintain your balance?
- Palpation (feeling) of the ankle joint and the surrounding soft tissues. This is used to locate the source of your pain. It can be painful but helps to formulate a diagnosis.
- Functional testing including walking, single leg balancing, hopping and running may be assessed, if appropriate.
As previously mentioned, lateral ankle ligament sprains have been shown to become chronic and persistent in up to 40% of cases (Golano et al., 2016). It is therefore critical that a timely and accurate diagnosis be made to ensure the most effective treatment is selected for you.
Other ankle pathologies are often associated with lateral ankle ligament sprains, causing recurrent sprains or perpetuating your symptoms. Diagnostic imaging is required to assess the presence of ankle pathology and to understand the level of injury present (partial or full ligament ruptures can be visualised as well as the surrounding soft tissues).
Ankle pathologies affecting lateral ankle ligament sprains include:
- Ankle impingement. Previous ankle trauma can result in the development of either a bony prominence on the talus bone or a soft tissue mass within the ankle joint. This can become impinged (pinched), resulting in joint pain and instability, increasing the risk of further lateral ankle ligament sprains.
- Sinus tarsi syndrome
- Ankle joint osteoarthritis
- Old ankle fractures
Diagnostic imaging options:
Diagnostic musculoskeletal ultrasound imaging
Diagnostic musculoskeletal ultrasound imaging is an excellent modality for assessing the swelling and inflammation associated with a lateral ankle sprain. It is capable of dynamically assessing the lateral ankle ligaments during movement (Singh et al., 2016), and visualising the extent of the ligamentous injury. The scan will reveal if there is a partial or complete ligament tear. Research has shown that diagnostic musculoskeletal ultrasound imaging is a highly effective and appropriate imaging tool to assess lateral ankle ligament sprains (Cho et al., 2016) and is capable of visualising swelling and inflammation (a condition known as synovitis) associated with lateral ankle ligament injury.
At Complete our team of clinicians are qualified as both physiotherapists and musculoskeletal sonographers. During your initial assessment your clinician will undertake a detailed clinical assessment including a diagnostic ultrasound scan. If you would like more information or would like to book an appointment please contact us on 0207 4823875 or email injections@complete-physio.co.uk.
Magnetic resonance imaging (MRI)
Diagnostic ultrasound imaging is able to provide all the information needed to diagnose a lateral ankle ligament injury however, an MRI may be requested if your clinician believes you may have injured your ankle joint or the talus bone (specifically an injury called an osteochondral defect). Patients with claustrophobia often find this process challenging. An MRI scan is expensive and time consuming compared to an ultrasound scan. MRI images consists of a series of images which create a highly detailed 3D image allowing for visualisation of your injury, resulting in an accurate diagnosis. MRI is often used to assess for ankle impingement, sinus tarsi syndrome and joint pathologies in the foot and ankle.
How do we treat lateral ankle ligament sprains?
Lateral ankle ligament sprains are often successfully treated with conservative management, often overseen by a physiotheraist.
Physiotherapy intervention used to rehabilitate a lateral ankle ligament sprain includes:
- Advice on activity modification.
- Balance and stability exercises to increase proprioception of the ankle.
- Ankle joint stretching exercises.
- Ankle strengthen exercises, including calf raises.
- Ankle bracing or physiotherapy taping to support and manage symptoms.
- Your clinician may use soft tissue massage techniques or ankle joint manipulations to increase ankle joint movement and help you to manage your pain and symptoms.
Here are a few tips and tricks you may wish to try yourself:
- Avoid aggravating your symptoms. Avoid walking on uneven surfaces, running or jumping.
- Use an ankle support. This will help to support the ankle reducing movements that may aggravate your symptoms.
- Calf strengthening exercises such as heel raises can help strengthen your ankle muscles and stabilise your ankle. As seen in the below image.
- Practice standing on one leg. Balance training is an important aspect of ankle stability and will help reduce your symptoms.
- Over-the-counter oral medication such as paracetamol or ibuprofen or a topical anti-inflammatory gel such as Voltarol can be effective at reducing pain. Talk to your pharmacist before taking medication.

What if conservative management does not work?
As previously mentioned, 10% of patients suffering from lateral ankle ligament sprains fail to improve with conservative management. If this is the case for you, then injection therapy may be appropriate for you.
Ultrasound-guided corticosteroid injection
An ultrasound guided corticosteroid injection may be useful if your symptoms remain persistent for over three months, are affecting your sleep or stopping you from completing your physiotherapy rehabilitation. The main reason for chronic ankle pain following an ankle sprain is ‘synovitis’ or lateral ‘gutter’ impingement.
Corticosteroid is a powerful, injectable anti-inflammatory medication that is routinely used to reduce pain and inflammation associated with musculoskeletal injury. A corticosteroid injection provides a period of pain relief allowing for a ‘window of opportunity’ for you to rehabilitate your ankle effectively. Research has revealed a combination of corticosteroid and physiotherapy results in significantly better outcomes. At Complete we recommend a course of rehabilitation start within two weeks after a corticosteroid injection.
At Complete all injection techniques are performed under ultrasound guidance. Ultrasound guided injections have been shown to be less painful and better tolerated by patients. They have less post injection complications and are significantly more accurate in hitting the intended target than Landmark guided injections.
During an ultrasound-guided injection a needle is guided directly to the source of your symptoms using an ultrasound machine. Corticosteroid injections are routinely combined with a short-acting local analgesic to enhance comfort during the procedure.
Complete clinicians are highly experienced in assessing and treating sinus tarsi syndrome. Our highly skilled team of professionals are fully qualified independent prescribers, physiotherapists, musculoskeletal sonographers and injection therapists. On your initial visit your clinician will provide an accurate diagnosis, prescribe the most appropriate medication for you and complete an ultrasound-guided injection all within the same session. You do not need a GP to refer you. You can simply self-refer directly into our same day service.
If you would like more information or would like to book an appointment please contact us on 0207 4823875 or email injections@complete-physio.co.uk.


Leave A Comment