Degenerative Disc Disease
Prices are inclusive of assessment, ultrasound scan and ultrasound guided injection
What’s Degenerative Disc Disease (DDD)
Degenerative Disc Disease (DDD) is a very common cause of both lower back and neck pain. It mainly affects the lumbar (lower back) and cervical (neck) areas of the spine. Though it can also present in the thoracic (mid-back) region.
The main treatments for DDD include medication, activity modification, rehabilitation, and physiotherapy. For those who do not experience sufficient relief, guided spinal injections (such as cortisone, also known as steroid and corticosteroid injections) is the next best option. Surgery is typically reserved for cases where other treatments have failed, with surgery reserved for cases where other treatments have failed.
Despite its name, DDD is not technically a disease but more of a sign the spine is going through some age related changes. By the age of 40, most people experience some form of “wear and tear” on their spinal discs, which is considered normal. Often, this degeneration happens without causing pain, and many people are unaware it has occurred.
As we age, the discs in our spine, which serve as cushions between the vertebrae, begin to lose water content, becoming drier and thinner. This process can lead to gradual disc deterioration.
In this article, we’ll guide you through the following points:
- Understanding the anatomy of the spine and its relationship to degenerative disc disease.
- The common causes and symptoms of DDD in the lumbar and cervical regions.
- How degenerative disc disease is diagnosed.
- Various treatment options to help you manage this condition and maintain an active lifestyle including guided spinal injections
Spine Anatomy and Disc Function in DDD
The spine is made up of a column of bones called vertebrae, which are divided into three regions: the cervical (neck), thoracic (upper back), and lumbar (lower back). There are 33 vertebrae in total, and between each vertebra is a soft disc that acts as a shock absorber for the spine and prevents the vertebral bones from rubbing against one another.
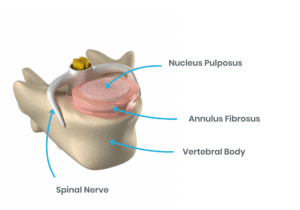
Each disc has a tough outer wall (the annulus), made up of dense fibrous bands that attach to the vertebrae and provide stability. The inner portion of the disc, called the nucleus, is gel-like and adjusts its shape to help distribute the pressure and load through the spine.
Maintaining enough space between the vertebrae is crucial for allowing normal spine movement and ensuring the spinal nerves pass freely through the spinal canal.
Causes of Degenerative Disc Disease
As we age, the water content in our discs diminishes. Discs that were once 80% water at birth begin to dry out, reducing their height and cushioning ability. This leads to less space between vertebrae and reduced shock absorption properties.
If the disc space becomes too narrow, additional pressure is placed on the vertebrae, potentially resulting in bone spurs (osteophytes) or even osteoarthritis (spondylosis). In some cases, reduced disc space can also compress spinal nerves, causing symptoms like cervical radiculopathy LINK (in the neck) or lumbar radiculopathy/sciatica LINK (in the lower back), which may present as weakness, numbness, or shooting pain in the arms or legs.
Degenerative changes in the discs also increase the risk of small disc tears, which further compromise disc function.
Risk Factors for DDD
In addition to age, several factors can accelerate disc degeneration or increase the risk of developing DDD:
- Obesity
- Heavy lifting or repetitive strain
- Smoking
- Previous injuries (e.g., falls, road traffic accidents)
- Family history
Secondary Conditions Linked to DDD
Disc degeneration can contribute to or accelerate the development of other spinal conditions, such as:
- Herniated Disc: The disc may bulge or rupture, placing pressure on surrounding nerves.
- Spinal Stenosis: A narrowing of the spinal canal that compresses the spinal cord or nerve roots.
- Spondylolisthesis: A condition where one vertebra slips forward over another due to joint and disc degeneration.
- Degenerative Scoliosis: Uneven degeneration can cause the spine to develop a sideways curvature over time.
Because these conditions often produce similar symptoms, it’s essential to seek a professional diagnosis.
Symptoms of Degenerative Disc Disease
The severity of symptoms varies widely between individuals. Some may have significant disc damage but only mild discomfort, while others with minimal degeneration may experience intense pain.
Common symptoms include:
-
Lumbar Spine Symptoms (Lower Back):
- Aching lower back pain, sometimes with sharp, stabbing sensations.
- Pain radiating into the legs and buttocks –
- “Seizing” or “locking up” sensations in the back – Muscle spasms
- Pain that worsens with prolonged sitting, bending, or twisting.
- Numbness, tingling, or weakness (in more severe cases) in the legs or feet.
-
Cervical Spine Symptoms (Neck):
- Neck pain, sometimes extending to the shoulders or arms.
- Numbness or tingling in the hands or arms.
- Stiffness and difficulty turning the neck.
- Symptoms exacerbated by prolonged sitting, such as working at a computer.
- Weakness in the arms or hands in more severe cases.
Diagnosing Degenerative Disc Disease
Diagnosing DDD can be challenging due to its gradual onset and the overlap of symptoms with other spinal conditions. Although sciatica or cervical radiculopathy can often be diagnosed based on symptoms, confirming that these issues are caused by disc degeneration typically requires an MRI scan.
Assessment and Imaging for DDD
At Complete Injections, our specialists take a comprehensive approach to diagnosis. This includes:
- A detailed medical history, including an account of your injury, symptoms, and daily activities.
- A thorough physical examination assessing spinal range of motion, muscle strength, sensation, reflexes, and posture.
Imaging techniques may also be recommended:
- X-rays: While X-rays cannot show soft tissues, they can reveal bone spurs, fractures, and reduced disc space.
- Magnetic Resonance Imaging (MRI): The best option for visualising soft tissues like discs, an MRI can show disc shrinkage, nerve compression, or spinal canal narrowing.
- Computed Tomography (CT) Scans: These scans are useful for providing detailed images of bone structures and may be used if MRI is not suitable.
If you would like to book in for a guided spinal injection, it is ideal to have had an MRI scan within the last 6 months, and preferably not older than one year. If needed, we may ask you to repeat the MRI, and our specialists can arrange this for you.
Treating Degenerative Disc Disease
Effective management of DDD often involves a combination of treatments to alleviate pain and improve function.
Physiotherapy for Degenerative Disc Disease
Physiotherapy plays a central role in conservative management, combining pain relief techniques with exercises to improve your mobility, strength, and posture.
If you have not yet tried conservative measures, we recommend booking an appointment with one of our expert physiotherapists, who can guide you through various treatment options such as pain relief techniques and exercises. They can also assess if an injection is appropriate and, if needed, refer you for an MRI.
Your physiotherapist will work with you to create a personalised treatment plan that may include:
- Pain relief strategies such as acupuncture, manual therapy, massage and activity modification and pacing techniques
- Stretching and mobility exercises
- Strengthening and core stability work such as clinical Pilates
- Functional and activity-specific rehabilitation
- Posture and movement re-education
Pain Management Options
In addition to physiotherapy, over-the-counter medications like nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and inflammation. For more severe pain, a muscle relaxant or prescribed painkiller may be necessary. Always consult a medical professional before taking any medication. Our specialist sports medicine consultants will be able to prescribe painkillers where appropriate if required, and this can help manage your symptoms effectively.
Spinal Injections for Degenerative Disc Disease
If your back or neck pain is severe enough to stop you from performing your normal daily activities, and conservative measures have not alleviated your symptoms, you may benefit from having an ultrasound guided spinal injection.
At Complete Injections, we work with a leading spinal specialist Dr. Matteo Bernardotto, a Consultant in Musculoskeletal Sport and Exercise Medicine who offers this service to Complete patients.
A combination of local anaesthetic and steroids is injected into the affected nerve, disc or joint to reduce inflammation and pain.
The location of your symptoms and the exact cause of your pain will determine the type of spinal injection that you will require.
The most common injections for DDD are:
Injections should not be used as a stand alone treatment and should always be followed by a structured physiotherapy program for long-term improvement. It is not a ‘quick fix’ but provides patients with good pain relief to give them a ‘window of opportunity’ to be able to take a more active part in their rehabilitation. Spinal injections can be particularly effective in providing rapid pain relief, especially from night pain. This allows for improved sleep, which supports better healing and enhances overall mental wellbeing and recovery.
Patients are generally encouraged to resume physiotherapy about one week after an injection to maximise recovery, but this can vary. Your specialist will provide specific guidance based on your individual condition.The pain relief from these injections last anywhere from a few weeks to several years, depending on the individual.
It is important to note that patients must have an up-to-date MRI scan (within the last 6 months ideally) before undergoing a spinal injection procedure, to ensure an accurate diagnosis and effective treatment.
Additionally, patients will be required to fill out a screening form to assess their eligibility for any spinal injection procedure. This helps us ensure your treatment is tailored to your specific needs and ensures the best possible outcomes.
Spinal Injections are carried out at our Kentish Town Clinic.
Spinal Surgery
Surgery is generally considered a last resort, typically only recommended for severe cases where conservative management, including injection therapy, has failed. This might be necessary if:
- You experience significant pain that interferes with daily life.
- You have severe weakness, numbness, or difficulty walking.
- Your pain impacts your sleep and mental health.
If surgery is needed, we can refer you to an experienced spinal surgeon, who we trust and work closely with and who will ensure you are given the best possible care. We will continue to follow your progress both pre and post op so that you have a smooth and seamless recovery journey.
If you would like to discuss your symptoms or explore treatment options for spinal injections or degenerative disc disease treatment, please contact us to book a consultation with one of our experienced specialists.
Ultrasound Guided Injection
Complete Injections is a highly specialised ultrasound guided injection service created to provide fast access to pain relieving injections for a wide range of musculoskeletal conditions delivered by our team of experts.
Self-referral accepted
We do not need a doctor to refer you
Minimal waits
We can usually see you within 24-48 hours
Excellent self-pay rate
From £230 including assessment, ultrasound guided injection and report
Highly experienced clinicians
We perform hundreds of injections every year
Convenient central London locations
ULTRASOUND GUIDED INJECTION ONE STOP SHOP FEES
- Same Day Consultation (subject to availability).
- Ultrasound scan and musculoskeletal assessment.
- Ultrasound Guided Injection.
- Report of assessment and scan findings and details of injection.
- All included for total fee: £230 cortisone injection, (advanced procedures are £250).
- A comprehensive range of injection procedures for musculoskeletal conditions are offered.
- All injections are performed by highly experienced advanced physiotherapists dual trained as physiotherapist and musculoskeletal sonographer.
- All are qualified as independent prescribers to allow them to screen you for any possible medicines interactions and select the most appropriate medication for your injection.
- All hold full qualifications in diagnostic ultrasound and injection therapy of peripheral musculoskeletal disorders.
Clinical Director
Chris is one of the few physiotherapists in the country to also be a fully trained as a musculoskeletal sonographer and uses diagnostic ultrasound to diagnose muscle, ligament, tendon, joint and nerve problems. He has been using diagnostic ultrasound…
Clinical Director
David is one of the pioneers of physiotherapists performing ultrasound guided injections. With 20 years of clinical experience as a chartered physiotherapist specialising in musculoskeletal care, David is clinical director at Complete Physio Ltd, with…
Injection Therapist
Luke is a highly specialised advanced level physiotherapist with a broad understanding of musculoskeletal health care. He qualified as a Physiotherapist in 2007 and has a wealth of experience working in both the NHS and privately settings.




