FROZEN SHOULDER TREATMENT
Our one-stop shop ultrasound guided injection clinic making access to pain relieving injections as easy as possible for patients whilst offering the highest levels of expertise and patient care.
FROZEN SHOULDER TREATMENT
Our one-stop shop ultrasound guided injection clinic making access to pain relieving injections as easy as possible for patients whilst offering the highest levels of expertise and patient care.
What is a frozen shoulder?
Frozen shoulder is a painful condition that causes pain and stiffness in the shoulder joint. It affects people between the ages of 40-60 years old (women more than men) and often starts for no obvious reason. On occasion, it can develop after shoulder surgery or after a fall. At your first appointment, your clinician will be able to diagnose if you have a frozen shoulder, using clinical tests and by carrying out a diagnostic ultrasound scan. Frozen shoulder often does not respond well to physiotherapy or conservative treatment such as rest and/or painkillers. An ultrasound-guided injection has been shown to be the most effective treatment for frozen shoulder.
What are the symptoms of a frozen shoulder?
The symptoms of a frozen shoulder are:
- Excruciating pain and significant stiffness in the shoulder
- Pain that is getting worse and radiates down the arm
- Pain that wakes you at night
If this sounds like your pain, read on…
What other conditions can mimic a frozen shoulder?
If this does not sound like your pain there are other conditions that can mimic the pain of a frozen shoulder such as:
Frozen shoulder vs rotator cuff pain
Frozen shoulder causes significant pain and stiffness i.e., even if you had no pain, you could still not move your arm through a full range of movement, whereas rotator cuff pain is painful but there is less associated stiffness.
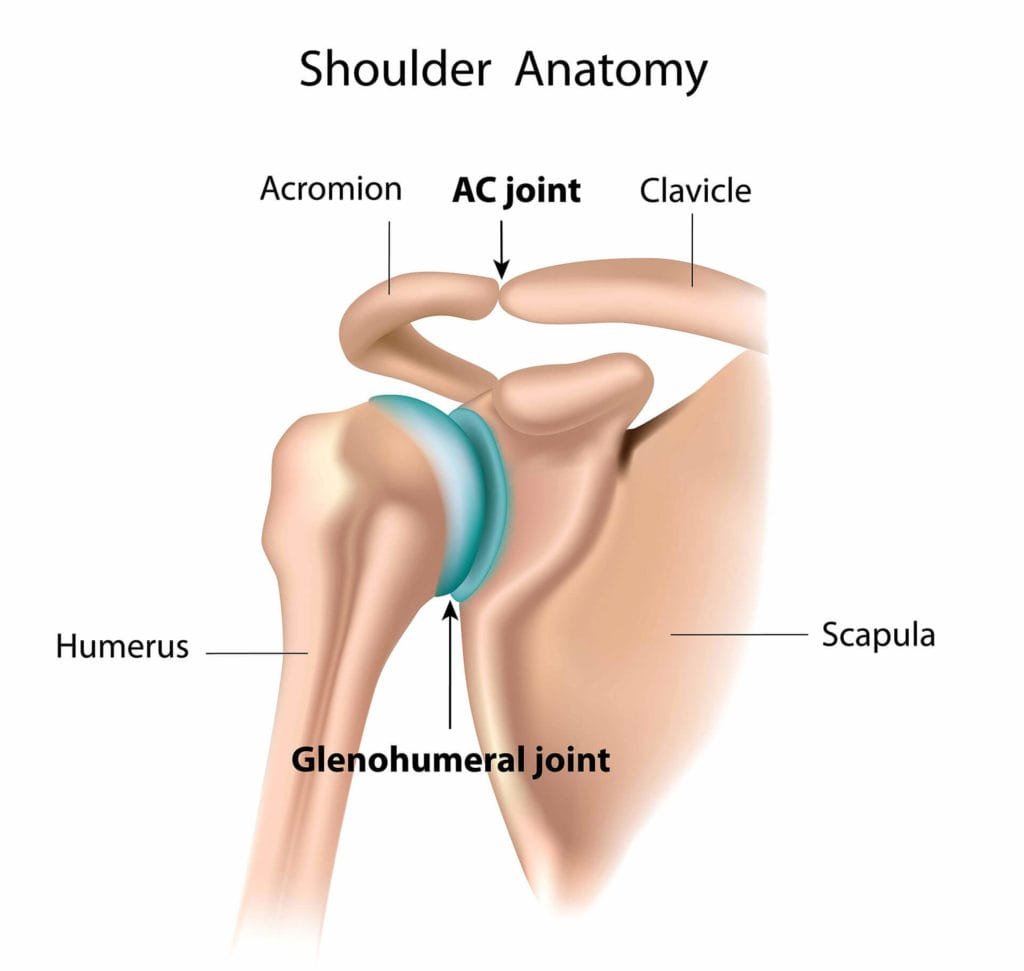
Anatomy
The glenohumeral (shoulder) joint is formed by the ball-shaped protuberance at the end of the humerus (long bone of the upper arm) and the shallow dish (called the glenoid fossa) positioned on the shoulder blade (scapula). These bones form the ball and socket joint known as the glenohumeral joint. This joint is capable of producing the wide variety of movements seen within the shoulder. It is this joint that is affected by adhesive capsulitis (frozen shoulder) which is the focus of this article.
Frozen shoulder is characterised by significant pain and progressive stiffness of the shoulder joint. More specifically, the capsule around the joint becomes inflamed and tight.
It is a very common cause of shoulder pain affecting between 2% and 5% of the population (Wu et al., 2017). It is unclear what causes frozen shoulder, but it is clear that this is a very painful and debilitating condition. Frozen shoulder often wakes people at night and even simple daily activities can be restricted and very painful.
Frozen shoulder has three distinct stages. The duration of each of these stages can vary from person to person and can last for several years before resolving.
The stages of frozen shoulder are:
- Stage one, known as the ‘painful’ stage. This stage can last several months, during which time the shoulder becomes increasingly stiff and painful.
- Stage two, known as the ‘stiff’ stage. During this phase, the shoulder remains very stiff resulting in limited function.
- Stage three, known as the ‘unfreezing’ or ‘thawing’ stage. During the ‘thawing’ phase the shoulder starts to ease, and movement becomes easier again. This can take many months or even years to resolve completely. Recent research shows that only 59% of patients regain full function within 4 years.
What are the risk factors associated with developing a frozen shoulder?
The mechanism underlying the development of frozen shoulder is still unknown, however, factors known to increase the risk of onset are as follows:
- Gender – women are more susceptible to frozen shoulder than men.
- Age – a majority of frozen shoulder cases occur in the 4th to 6th decade of life.
- Trauma – injury of the shoulder, including fractures, dislocations, rotator cuff tears, or surgery can all be associated with the onset of secondary frozen shoulder.
- Diabetes mellitus (type 1 and type 2)
- Over or underactive thyroid
- Cardiovascular disease.
How do you know if you have a frozen shoulder?
Frozen shoulder often starts insidiously but can also occur after trauma or injury. However, an insidious onset is by far the most common.
Symptoms of frozen shoulder include:
- Significant pain that is difficult to manage with over-the-counter pain medication, ice and physiotherapy.
- Pain that is affecting your ability to sleep or is regularly waking you at night.
- Increasing stiffness in the shoulder that is limiting your ability to raise your arm or perform activities of daily living such as dressing and undressing.
How is frozen shoulder diagnosed?

If you feel you may have a frozen shoulder it is recommended that you seek professional assistance as soon as possible. A diagnosis of frozen shoulder is made using clinical assessment by your clinician. A formal diagnosis is created by a combination of strength and range of movement testing.
Other pathologies that may present like a frozen shoulder need to be ruled out. These include:
- Glenohumeral joint osteoarthritis
- Acromioclavicular joint osteoarthritis
- Calcific tendinopathy
- Rotator cuff tendinitis/tendinopathy
- Subacromial bursitis
- Long head of bicep tendinitis/tendinopathy
If, after completing a clinical assessment your clinician is still unsure of your diagnosis you may be referred for an x-ray. This is to rule out other shoulder pathology which can present like frozen shoulder such as shoulder osteoarthritis.

X-ray is the gold standard imaging technique for assessing joint pathology including osteoarthritis or fracture. Your clinician may refer you to have a series of blood tests. Blood tests are used to rule out other pathologies such as systemic inflammation associated with rheumatoid arthritis. These are normally not required.
Although x-ray is an excellent modality for assessing joint pathology it is not capable of assessing the soft tissue inflammation often associated with this condition. This can be easily visualised using diagnostic ultrasound imaging.
All our clinicians are fully qualified musculoskeletal physiotherapists and sonographers. All our assessments are completed using a combination of clinical testing and a diagnostic ultrasound scan. The in-depth nature of our assessments results in a highly specific diagnosis and the development of an effective, individualised treatment approach.
How do we treat frozen shoulder?

Research has revealed that conservative management alone has limited value in the painful (first) stage of frozen shoulder. Physiotherapy for the management of frozen shoulder will include a progressive stretching home exercise program, manual techniques to mobilise your shoulder joint, and potentially acupuncture and taping.
It is not uncommon that the pain is too severe for you to engage in a course of physiotherapy. This is when an injection is advised to get the pain under control. An ultrasound-guided injection is a well-supported treatment modality for frozen shoulder and is recommended in the NICE guidelines.
Here are some top tips for treating frozen shoulder which may help:
- Modify your activities of daily living and try to avoid tasks that aggravate your pain. This could include taking regular breaks or dividing a task into smaller more manageable pieces.
- If you sleep on your side, we would suggest you lie on the unaffected side with a pillow under your painful arm. Alternatively, if you lie on your back then place the pillow under the back of your shoulder and under the painful arm.
- Start a gentle stretching program for your shoulder joint. Walking your fingers up a wall is a good way to start stretching the shoulder joint. It may be easier to stretch the shoulder after a hot shower/bath or by applying a hot water bottle.
- Over-the-counter medication can be effective at reducing pain. Discuss the use of medication with your pharmacist before starting treatment.
What if conservative management does not work?
Injection therapy
If your pain remains significant and is affecting your daily life, then injection therapy may be appropriate. Injection therapy is particularly effective in the following circumstances:
- If you are in significant pain, particularly pain that is waking you several times a night, then an ultrasound-guided injection is the treatment of choice. This is well supported in the medical literature.
- Pain that is stopping you from completing normal tasks such as washing and dressing, cooking or leisure activities.
- Pain that is limiting your ability to undertake physiotherapy rehabilitation.
During stage one, patients find it very difficult to gain any pain relief and even small movements aggravate the pain. Often once the pain is aggravated it takes several hours even days for the pain to settle again. Injections are used to reduce the pain and inflammation associated with frozen shoulder. This allows a ‘window of opportunity’ for you to stretch your shoulder effectively. Research has recommended that, for best results, a course of physiotherapy should be started within two weeks after receiving a shoulder joint injection.
The current evidence base has shown that injections completed under ultrasound image guidance are more accurate at delivering the medication to the shoulder joint, and more effective at reducing pain and increasing function than landmark guided injections (Daniels et al., 2018; Aly et al., 2015). Research has also revealed ultrasound-guided injections can significantly reduce pain associated with frozen shoulder, particularly in the short term. This can be of great benefit when combining injection therapy with physiotherapy.
At Complete Injections, all our clinicians are fully qualified at performing ultrasound-guided injections and are highly experienced in treating frozen shoulder. All injections are performed using ultrasound guidance. If you would like more information or would like to book an appointment, please contact us on 0207 4823875 or email injections@complete-physio.co.uk.
If you would like more information or would like to book an appointment, please contact us on 0207 4823875 or email injections@complete-physio.co.uk. Please note you do not need a GP referral, this is a self-referral service.

