‘What is best for me, a corticosteroid or a hyaluronic acid injection?
This a very common question we get asked at Complete and the answer is simpler than you might think. The answer comes down to a few simple variables.
In short, if you are experiencing significant levels of joint pain, have a swollen joint or have pain which is not joint related, then the fast-acting pain-relieving properties of corticosteroid make it the most appropriate injection for you.
If you have a confirmed diagnosis of osteoarthritis, are finding activities of daily living troublesome, and want to maintain optimum joint function for as long as possible the hyaluronic acid injections are indicated.
It is common for patients to experience flare-ups of pain from an osteoarthritic joint. For these patients, a combination of pain relief and joint preservation can be achieved by combining a corticosteroid injection with hyaluronic acid.
To understand whether corticosteroid or hyaluronic acid is best suited to your symptoms it is essential to answer some important questions:
- What is your diagnosis?
- What is a corticosteroid injection and what outcomes should you expect?
- Can your condition be treated with a corticosteroid injection?
- What is a hyaluronic acid injection and what outcomes should you expect?
- Can your condition be treated with a hyaluronic acid injection?
What is your diagnosis?

Corticosteroid injections and hyaluronic acid injections have been proven to be effective pain killers. However, they have the potential to offer very different outcomes. Each are best suited to a specific set of clinical criteria (more on this later). Before you can make an informed decision as to which injection option is best suited to you it is critical that an accurate and timely diagnosis is made.
No injection should be carried out without a formal diagnosis. At Complete, our team of highly specialised clinicians, combine both a full clinical assessment with diagnostic ultrasound imaging to provide you with an accurate diagnosis. Ultrasound is excellent for assessing soft tissues including muscles, tendons, and ligaments, as well as joint swelling. However, it is unable to see deep inside the joint itself. In some cases, if a diagnosis cannot be accurately made, you may be referred to an orthopaedic consultant or for an MRI. Once you have a definitive diagnosis your clinician will be able to discuss with you the pros and cons of each injection type.
What is a corticosteroid injection and what outcomes should you expect?
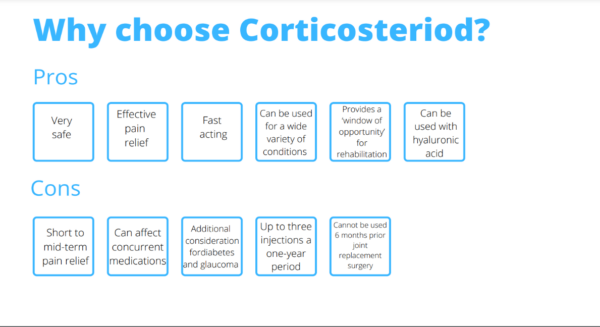
Corticosteroids are potent, injectable, anti-inflammatory medications which have been used as effective painkillers in musculoskeletal healthcare for decades. When injected, corticosteroid has the potential to rapidly reduce pain and swelling. The effects of corticosteroids can be felt as early as 6 hours after injection, although most people experience the maximum benefits within the first 2 weeks.
How long the beneficial effects of a corticosteroid injection will last is less predictable. Consensus in the research suggests significant pain relief lasting up to 3 months (Saunders., 2012). However, many people experience a much longer period of pain relief after an injection, while others find corticosteroids provide very short-term pain relief or none at all (although this is very rare).
Many patients are concerned about how many corticosteroid injections they can safely have. The consensus states that up to 3 injections can be carried out in one area each year MacMahon et al., 2009; Saunders., 2012; Simurina et al., 2019. For best outcomes, it is essential that after receiving a steroid injection the underlying cause of your pain is treated. A course of physiotherapy after an injection for a musculoskeletal problem is essential to ensure you achieve maximum benefit.
There are two main corticosteroids used in the UK. These are Depomedrone and Kenalog. Both medications are highly effective at controlling pain and swelling and stay within the body for an average of between 3-4 weeks before being removed by your kidneys.
Corticosteroids are prescription only medications which have the potential to affect patients who are taking other specific medications or have comorbidities such as diabetes or glaucoma, therefore only doctors and independent prescribers can prescribe and administer this medication. All clinicians at complete are fully qualified physiotherapists, musculoskeletal sonographers, and independent prescribers. This unique combination allows for fast effective pain relief without requiring a referral from a doctor.
To know more about contraindications surrounding corticosteroids and whether they are suitable for you please follow this link.
Can my condition be treated with a corticosteroid injection?

Corticosteroids are very effective at reducing pain and swelling in the short to mid-term. As previously discussed, a corticosteroid should be used as a ‘window of opportunity’ allowing you to address the underlying cause of your pain. We strongly recommend any injection be followed up by a course of physiotherapy.
Pain and swelling can originate from many different structures in the body however, the two most common causes are joints and bursa (fluid filled sacks used to reduce friction, often found next to tendons).
Below is a list of some of the most common conditions which respond well to corticosteroid injections. The list is by no means exhaustive. If you do not see your condition below, please feel free to contact Complete
on 020 7482 3875 or email injections@complete-physio.co.uk to talk to one of our clinical specialists. If you believe you are suffering from one of the below conditions, please click on the link to read more:
Shoulder conditions
- Frozen shoulder
- Osteoarthritis of the glenohumeral joint (ball and socket joint of the shoulder).
- Acromioclavicular joint pain
- Bursitis of the subacromial bursa
Hand and wrist conditions
- Osteoarthritis of the wrist
- Osteoarthritis of the thumb
- Trigger finger
- De Quervain’s tenosynovitis
- Carpal tunnel syndrome
Hip conditions
- Osteoarthritis of the hip joint
- Femoroacetabular impingement (FAI)
- Psoas bursitis
- Greater trochanteric pain syndrome
Knee conditions
Ankle and foot conditions
What is a hyaluronic acid injection and what outcomes should you expect?
The internal surface of a joint is covered by a smooth, friction reducing layer of articular cartilage. Articular cartilage provides the joint with friction free motion and protects the underlying bone surfaces from damage. Joints are surrounded by a joint capsule. The innermost layer of the joint capsule is called the synovial membrane. The synovial membrane secretes synovial fluid, which acts as a joint lubricant and in turn protects the articular cartilage. Both the synovial membrane and articular cartilage are richly supplied with hyaluronan receptor cells which bind to hyaluronic acid. The role of the hyaluronan cells, and the hyaluronic acid produced, is to provide lubrication and shock absorption. This is achieved due to its viscoelastic (thick and gooey) properties. The viscoelasticity of hyaluronic acid has a direct impact on the ability of the joint to lubricate itself. Simply speaking reduced viscoelasticity results in reduced lubrication. A joint which is poorly lubricated is more susceptible to articular cartilage damage which ultimately results in the onset of osteoarthritis (Altman et al., 2015; Cheng et al., 2014).
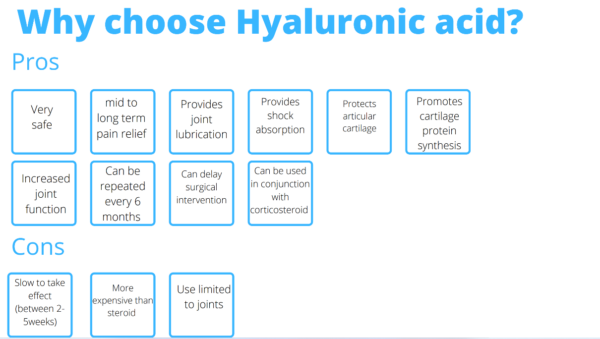
Injectable hyaluronic acid is a synthetic replication of this naturally occurring substance. Research has shown that supplementing an osteoarthritic joint with hyaluronic acid provides increased shock absorption and joint lubrication. It also has the ability to protect the articular cartilage, stimulate the production of protective proteins within the articular cartilage, and promote the development of subchondral bone growth (the layer of bone which lies immediately beneath the articular cartilage (Altman et al., 2015).
There are two industry leading variations available Ostenil plus and Durolane both of which vary in viscosity and volume. Hyaluronic acid is categorised as a ‘medical device’ and is therefore not a prescription only medication. However, all joint injections are completed using a local anaesthetic (Lidocaine) which is a prescription only medication.
Research reports that the benefit of hyaluronic acid injections is long-term pain relief and increased joint function. These benefits have been shown to last for up to one year (of course this can vary between individuals) and can be used safely on a six monthly basis without any deleterious effects to the joint. Research states that hyaluronic acid is a safe product with very few side effects and can be used to delay the need for surgical intervention (Altman et al., 2015; Baron et al., 2018; Maheu et al., 2019; Bahrami et al., 2020).
Hyaluronic acid does not have an immediate effect on either pain or function levels. The benefits can take between 2 to 5 weeks to appear, so a little patience is required.
Can my condition be treated with a hyaluronic acid injection?
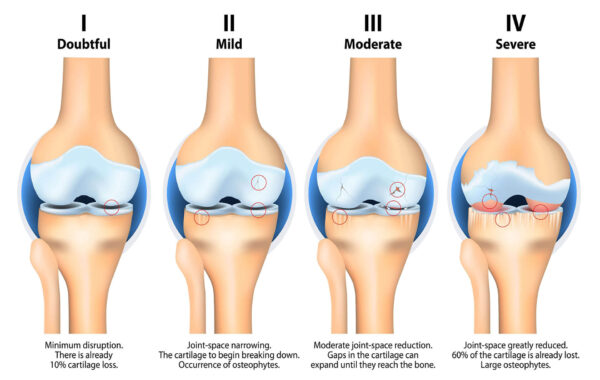
Hyaluronic acid injections are a safe and effective way to increase the function of an osteoarthritic joint as well as reduce pain (Baron et al., 2018; Maheu et al., 2019; Bahrami et al., 2020). Research reports excellent outcomes for patients suffering from osteoarthritis across the board, but the best results are observed in patients with the following profiles (Maheu et al., 2019):
- Mild to moderate levels of osteoarthritis (diagnosed on X-ray)
- Age of up to 60
- Joint pain which requires multiple pain medications to control
- Significant levels of pain and dysfunction
- No joint swelling
Below is a list of some of the most common conditions treated using hyaluronic acid injections. If you have any queries or do not see your condition listed, please feel free to contact Complete to speak to one of our clinical experts.
So which injection is right for me?

As we have seen corticosteroid and hyaluronic acid injections work in very different ways and have different perceived outcomes. The choice of injection depends on your diagnosis and what you want from the injection.
Hyaluronic acid is primarily used to treat joint pathology, and in particular osteoarthritis. The goal of hyaluronic acid is to lubricate and protect a joint. It is not designed to provide quick pain relief. However, if you have been diagnosed with bursitis, nerve entrapment or acute joint pain which is associated with swelling then a corticosteroid injection will serve you best.
The tables below help to summarise the key pros and cons of both corticosteroid and hyaluronic acid injections.
Can corticosteroid and hyaluronic acid be injected at the same time?
In short, yes! Corticosteroid can be combined with hyaluronic acid for patients suffering from chronic osteoarthritic joint pain who are experiencing an acute flare of pain and swelling.
By combining corticosteroid with hyaluronic acid, you can achieve the best of both worlds. The corticosteroid provides fast-acting pain relief which bridges the gap whilst the hyaluronic acid takes effect.

If you would like more information about whether corticosteroid or hyaluronic acid is right for you, please contact one of our clinical specialists on 020 7482 3875 or email injections@complete-physio.co.uk.
References:
Altman, R.D., Manjoo, A., Fierlinger, A., Niazi, F. & Nicholls, M. 2015, “The mechanism of action for hyaluronic acid treatment in the osteoarthritic knee: a systematic review”, BMC musculoskeletal disorders, vol. 16, no. 1, pp. 321.
Saunders, S., FCSP & Longworth, S. 2012, Injection techniques in musculoskeletal medicine: a practical manual for clinicians in primary and secondary care, 4th edn, Churchill Livingstone Elsevier, Edinburgh.


