What is osteoarthritis (OA) of the thumb (also known as first carpometacarpal joint arthritis)?
Osteoarthritis of the thumb is a chronic condition causing pain, stiffness and occasional clicking and swelling in the joint at the base of thumb (also known as the carpometacarpal or CMC joint). Simple daily tasks such as chopping food can become painful and difficult. The prevalence of thumb osteoarthritis increases with age. It often develops overtime, for no apparent reason, starting with mild pain and stiffness.
There is no specific cure for osteoarthritis, but there are effective options available to reduce your pain and improve your function. Resting from the aggravating factors, a thumb spica, painkillers/anti-inflammatories and physiotherapy all help to provide pain relief and improve mobility and strength. Ultrasound guided steroid injections can provide rapid pain relief. Injections should always be followed up with a course of physiotherapy which may involve exercises and/or hands-on/manual therapy and/or acupuncture. Hyaluronic acid injections provide a suitable alterative to steroid injections, and are also used to lubricate the joint to help mobility and reduce your pain. Joint replacement surgery is reserved for those in severe pain that have not improved with injections and physiotherapy input.
What are the symptoms of osteoarthritis (OA) of the thumb?
The symptoms of osteoarthritis of the thumb are:
- Swelling, stiffness and tenderness at the base of your thumb
- Pain and weakness when pinching or gripping objects, particularly between your thumb and index finger (pincer grip).
- Enlarged, thickened or bony appearance of the joint at the base of your thumb
If this sounds like your pain, read on below…
What other conditions can mimic osteoarthritis (OA) of the thumb?
If this does not sound like your pain there are other conditions that can mimic the pain of osteoarthritis thumb, such as:
- Carpal tunnel syndrome
- DeQuervain’s tenosynovitis
- Osteoarthritis of the wrist
- Triangular fibrocartilage complex (TFCC) tear
- Scapholunate ligament injury
Osteoarthritis (OA) of the thumb vs DeQuervain’s tenosynovitis
Thumb osteoarthritis causes localised pain, stiffness and swelling around the joint at the base of the thumb. However, DeQuervain’s disease also causes pain and swelling but is located towards the wrist crease on the thumb side of the wrist. Both conditions are aggravated by thumb movements and gripping and carrying. Thumb Osteoarthritis is more common in those over 50 years old, whereas DeQuervain’s disease is more common in younger men and women, particularly women immediately postpartum.
Anatomy
The joint at the base of your thumb is known as the first carpometacarpal (CMC) joint. It connects the thumb to your wrist and is critically important in the production of the complex series of movements possible by the thumb. The first CMC joint is created by the articulation of the trapezium bone (one of the small carpal bones of the wrist) and the metacarpal bone of the thumb (the first long bone at the base of your thumb). This joint is able to perform a series of movements due to its complex ‘saddle’ shaped morphology. The image below shows the location of the first CMC joint.

The first CMC joint is responsible for producing the following movements:
- Flexion (crossing your thumb across the palm of your hand) and extension of the thumb (moving your thumb away from palm).
- Abduction (bringing your thumb towards your fingers) and adduction of the thumb (separating your thumb away from your fingers).
- Opposition of the thumb. This is the movement that allows your thumb to make a circle of reach over to touch your little finger.
The first CMC joint is a common site for osteoarthritic change. This is due to the constant movement of the thumb throughout the day. A recent study revealed first CMC joint osteoarthritis is present in 2.2% of patients suffering from hand pain (Kwok et al, 2014).
Many risk factors are associated with the onset of first CMC osteoarthritis and include:
- Age – Prevalence of first CMC joint osteoarthritis increases significantly after the age of 50 (Sonne-Holm et al, 2006)
- Sex – Women are at a higher risk of first CMC joint osteoarthritis than men (Sonne-Holm et al, 2006)
- High body mass index has a direct correlation with osteoarthritic change at the first CMC joint
- Trauma – Previous injuries such as dislocations of the thumb can predispose the joint to osteoarthritis, thumb dislocations are common during sporting activities such as skiing
- Occupation – Some occupations require repetitive thumb movements (for example builders), repetitive thumb movements over many years can predispose the thumb to osteoarthritic change
- Sporting activities – Repetitive action during some sports, such as Tennis
Osteoarthritis is a progressive, degenerative condition caused when the thumb is exposed to prolonged periods of one or more of the above risk factors.
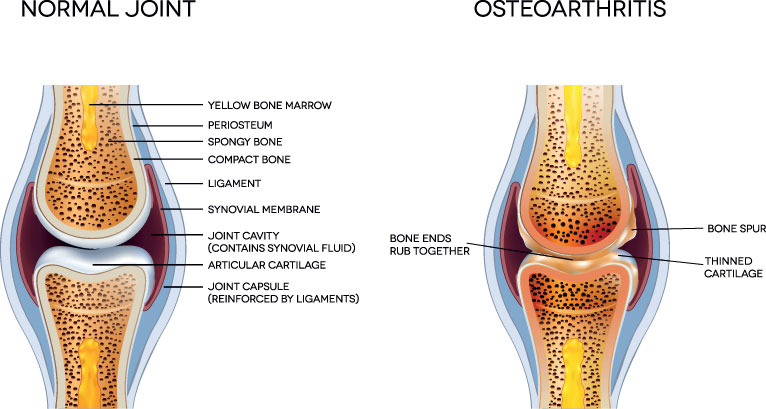
To allow fluid, frictionless movement and to provide a layer of protection the bones of the first CMC joint (trapezium and first metacarpal bone) are coated in a layer of articular cartilage. If the joint is subjected to repetitive periods of misuse, overuse or abuse this articular cartilage can be worn down. As time progresses the delicate bone surfaces, previously protected by the layer of cartilage, are exposed and rub together. As a result of this process the connective tissue within the joint space, known as the synovium, becomes irritated and inflamed causing synovitis. Synovitis is responsible for the sharp flareups of pain associated with osteoarthritis and has been proven to be associated with disease progression.
How do I know if I have osteoarthritis of the thumb?
Osteoarthritis is typically a slow progressive disease that can take many years to develop before becoming symptomatic. Symptoms are often intermittent initially causing low levels of pain but become more constant and painful as the disease progresses.
Symptoms of first CMC joint osteoarthritis include:
- Dull aching pain at the base of the thumb.
- Intermittent sharp periods of increased pain at the base of the thumb. Often associated with synovitis.
- Swelling at the base of the thumb.
- Clicking or cracking noises emanating from the thumb joint.
- Stiffness. Your joint movement may become reduced as osteoarthritis progresses.
- Thickened, enlarged base of the thumb. This is due to a change in joint shape which is associated with more significant cases of osteoarthritis and is known as joint deformation.
- Weakness in the thumb affecting gripping and pinching activities such as opening a door, opening a jar, shaking hands, turning a key.
How is osteoarthritis of the thumb diagnosed?
Obtaining a correct diagnosis of first CMC joint osteoarthritis is essential and informs the clinician of which treatment option would be most beneficial for you.
If you suspect you have osteoarthritis in your thumb you should seek professional advice. First CMC joint osteoarthritis is diagnosed using a combination of clinical testing (including range of movement and strength testing of the thumb) and diagnostic imaging (e.g. x-ray).
Your GP will often refer you for an x-ray if they suspect you have osteoarthritis. An x-ray is a highly effective diagnostic tool commonly used for assessing bone and joint health and is capable of assessing the severity of osteoarthritic change in an affected joint. Your GP may also request blood tests. These are used to rule out the presence of systemic inflammatory processes which can also cause thumb pain. Although x-rays are very good at showing the presence and severity of osteoarthritis they do not always correlate with pain and symptoms. Commonly patients experience pain and symptoms which feel more significant than is expected after reviewing x-ray findings. This is especially true during a flareup in pain. The below image shows an x-ray of the hand and wrist with the 1st CMC joint highlighted.

Diagnostic musculoskeletal ultrasound imaging is an evidence-based diagnostic tool commonly used for the assessment of first CMC osteoarthritis. Diagnostic ultrasound is highly sensitive at visualising bony irregularities associated with osteoarthritis and is excellent at observing inflammation associated with synovitis (Kaeley et al., 2020; Wakefield et al., 2000). The team of highly skilled clinicians at Complete are also qualified musculoskeletal sonographers, experienced in diagnosing first CMC osteoarthritis. During the assessment, your clinician will clinically assess your thumb and perform a diagnostic ultrasound scan of the area.
How do we treat osteoarthritis of the thumb?
The vast majority of patients respond very well to physiotherapy treatment using a combination of thumb stretches and strengthening exercises. Current evidence reveals that strength and flexibility are the most important factors in maintaining function and reducing pain in osteoarthritic joints. After your physiotherapist has assessed your thumb, they will provide you with an individualised progressive exercise program aimed at maintaining strength, flexibility and function. In some cases, your physiotherapist may also perform some manual release techniques which may involve manipulating your thumb to increase your range of movement. Your clinician may also suggest the use of a thumb splint. Splints are regularly used to limited painful movements whilst allowing you to continue using your thumb.

Here are a few tips you may like to try yourself:
- Avoid painful activities as much as possible. If this is not possible try to modify these activities as best as you can. This may include taking regular breaks, changing hand and wrist positioning, or using a splint.
- Try gentle thumb stretches. Flexibility has been proven to reduce the effects of osteoarthritis.
- Practice grip strengthening exercises. This can be done by squeezing a ball, rolled up socks, or a tennis ball.
- Try using assistive aids such as jar openers or tap turners to gain extra purchase during activities of daily living.
- Over-the-counter oral medication such as paracetamol or using a topical anti-inflammatory gel such as Voltarol can be effective at reducing the pain associated with osteoarthritis. Please ask your pharmacist first.
What if conservative management does not work?
If your thumb pain remains persistent even after a course of physiotherapy or is affecting your daily life, then an ultrasound-guided steroid injection may be suitable for you.
A corticosteroid is a highly effective injectable, anti-inflammatory medication that is routinely used to treat the pain and inflammation associated with osteoarthritis. Corticosteroids are particularly effective when your pain is affecting the following:
- Affecting your ability to sleep or waking you up at night.
- Stopping you from completing your normal activities including cooking, dressing and cleaning as well as leisure activities including gardening or racquet sports.
- Affecting your ability to take part in your physiotherapy treatment.
Research has shown that corticosteroid injections are more effective and more accurate when performed under the guidance of ultrasound imaging. Real-time ultrasound imaging is used to achieve precise needle placement.
Hyaluronic acid is a synthetically manufactured medication which mimics the natural lubrication of the joint. Current evidence shows it is an effective alternative to corticosteroid injection for reducing pain and inflammation in arthritic joints. Hyaluronic acid injections are completed under ultrasound guidance using the same procedure as a corticosteroid injection.
At Complete Injections, all of our clinicians are experienced in performing ultrasound-guided injections. At your initial assessment, your clinician will be able to assess your thumb and if appropriate perform an ultrasound-guided injection all within your first visit. Complete are able to perform a same day service for all ultrasound-guided injections. You do not need to be referred by a GP or bring a prescription. Your clinician is able to select and prescribe the most effective medication for you prior to the injection. For the best possible results after any ultrasound-guided injection, we recommend a course of physiotherapy, starting within 2 weeks after the injection. Injections provide a ‘window of opportunity’ allowing you to rehabilitate your thumb joint effectively without pain.
Other Wrist & Hand conditions:
Osteoarthritis (OA) wrist joint
Trigger Finger/thumb
Carpal Tunnel Syndrome
Triangular fibrocartilage complex (TFCC)
De Quervain’s Tenosynovitis
Scapholunate ligament injury (pain in the wrist)
If you would like more information or would like to book an appointment please contact us on 0207 4823875 or email injections@complete-physio.co.uk.
References
KAELEY, G.S., BAKEWELL, C. and DEODHAR, A., 2020. The importance of ultrasound in identifying and differentiating patients with early inflammatory arthritis: a narrative review. Arthritis research & therapy, 22(1), pp. 1-10.
Out us KWOK, W.Y., KLOPPENBURG, M., MARSHALL, M., NICHOLLS, E., ROSENDAAL, F.R. and PEAT, G., 2014. The prevalence of erosive osteoarthritis in carpometacarpal joints and its clinical burden in symptomatic community-dwelling adults. Osteoarthritis and Cartilage, 22(6), pp. 756-763.
SONNE-HOLM, S. and JACOBSEN, S., 2006. Osteoarthritis of the first carpometacarpal joint: a study of radiology and clinical epidemiology. Osteoarthritis and Cartilage, 14(5), pp. 496-500.
WAKEFIELD, R.J., GIBBON, W.W., CONAGHAN, P.G., O’CONNOR, P., MCGONAGLE, D., PEASE, C., GREEN, M.J., VEALE, D.J., ISAACS, J.D. and EMERY, P., 2000. The value of sonography in the detection of bone erosions in patients with rheumatoid arthritis: A comparison with conventional radiography. Arthritis & Rheumatism, 43(12), pp. 2762-2770.


Leave A Comment