To understand what platelet rich plasma (PRP) is, we first need to know what platelets and plasma are. Both platelets and plasma are found in blood.
The four components of blood are:
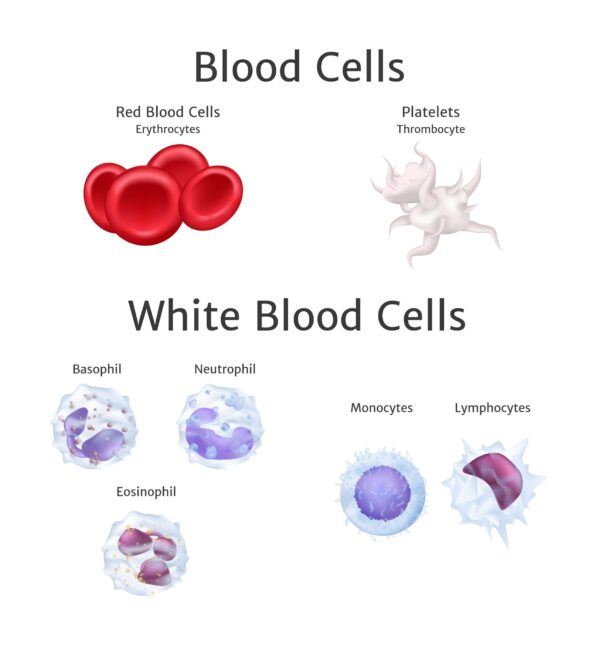
- Red blood cells. Red blood cells contain haemoglobin which binds to oxygen molecules. Oxygen rich red blood cells are transported throughout the body to deliver oxygen wherever it is required.
- White blood cells. White blood cells are produced in bone marrow and are an important part of the immune system. They are found both in the blood stream and the lymphatic system.
- Plasma. Plasma makes up about half of the fluid content of the blood. Its role is to transport red and white blood cells as well as platelets, proteins and hormones around the body. Waste products are also deposited into plasma to be removed from the blood stream, and ultimately the body.
- Platelets. Platelets are small cells found within the plasma. The normal platelet count in blood ranges from 150,000/uL to 350,000/uL. The job role of platelets is to regulate wound healing. Platelets achieve this due to the many bioactive factors found within their makeup. Cells found within platelets promote wound healing and include cytokines (specialist protein cells designed to maintain a healthy immune system), clotting factors (cells capable of stimulating cell proliferation) and platelet derived growth factors (PDGF) (molecules which stimulate wound healing). PDGFs promote the growth of soft tissue, blood vessels and bone as well as inhibiting cell death (apoptosis). Furthermore, calcium and adenosine (aiding the aggregation of platelets), dopamine (a neurotransmitter used to regulate blood pressure and heart rate), and serotonin and histamine (increases capillary permeability and activates macrophages) are all found within platelets. These cells also play a pivotal role in wound healing (Foster et al., 2009).
What role do platelets play in the healing process?
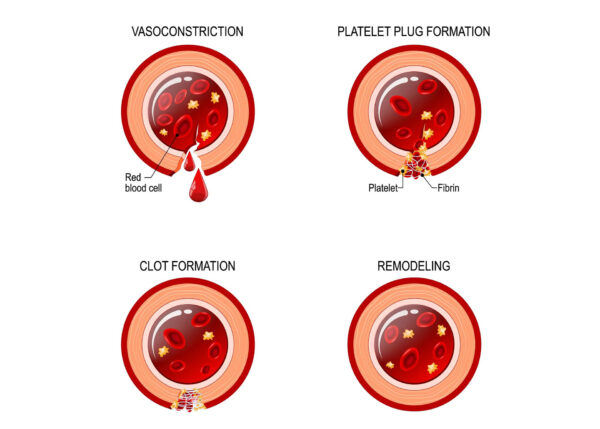
The healing process can be divided into three parts – inflammation, proliferation and remodelling. Platelets, in particular PDGFs, play a crucial role in the inflammatory stage, although their presence is felt throughout.
During the inflammatory phase platelets are stimulated to initiate wound healing. Foster et al., (2009) report that platelets achieve this in a variety of ways:
- Clotting occurs via the stimulation of cytokines and growth factors. Clotting is an important part of the healing process. It provides a temporary structure to the injured tissue and acts as a location for other wound healing cells to congregate.
- Increased permeability of local capillaries is promoted by the release of histamine and serotonin. This increases access to the wound site to allow healing to occur.
- PDGFs promote the activation of fibroblasts to produce collogen (a key component of connective tissue) as well as stimulate the production of extracellular matrix (provides structural support for soft tissue). The extracellular matrix is capable of withstanding the compressive forces that healthy tissue is routinely subjected too.
- Macrophages (white blood cells responsible for cleaning up dead cells and stimulating an immune response) are stimulated to migrate to the site of injury.
What is platelet rich plasma (PRP)?
For the body to maintain healthy tissue, a fine balance between damage and restoration (a process known as homeostasis) is required (Filardo et al.,2013). Homeostasis can be affected in many ways, all of which ultimately lead to degenerative changes. Degenerative change within a joint is known as osteoarthritis; degenerative change within tendons is known as tendinopathy. Treatment using PRP is a safe and effective process designed to stimulate healing and tissue regeneration.
As previously described platelet concentrations within the blood stream range between 150,000/uL to 350,000/uL. However, after blood is subjected to the PRP process (more on this later) platelet counts are found to be significantly higher ranging up to 1,000,000 to 2,000,000/uL. This results in 3 to 6 times greater levels of growth factors (Foster et al., 2009; Raeissadat et al., 2015). The growth factor ratios found within PRP have been shown to remain true to the physiological proportions observed in normal blood but are more concentrated (Filardo et al.,2013). The concentrated levels of growth factors found within PRP have been reported to facilitate superior wound healing.
In conclusion PRP has been shown to have positive effects on the healing process via the following mechanisms:
- PRP is autologous (the PRP is produced from the recipient’s own blood) it is therefore completely biocompatible making it very safe with minimal side effects.
- PRP contains highly concentrated levels of growth factors which stimulate the healing process.
- PRP forms a “fibrin scaffold” which allows the extracellular matrix to form. This also acts as a migration point for other pro healing cells to migrate to.
(Zhou et al., 2015)
How is PRP harvested?
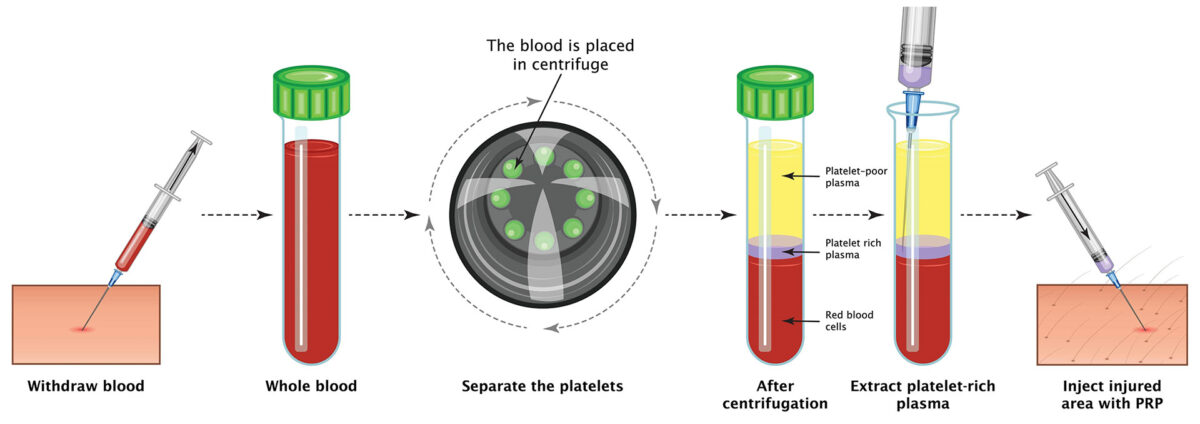
PRP is harvested directly from you own body. A small needle is inserted into one of the large veins in the crook of your elbow and a small amount of blood is removed (typically 15ml). This process is the same as when having a blood test.
Once collected, the syringe containing the blood sample is placed into a centrifuge machine which spins at high speed. During spinning the blood molecules are separated. The red and white blood cells are larger than the plasma cells (7-15um vs 2um in diameter) and so are forced to the bottom of the syringe. This leaves the plasma component sitting on top (Pauloni et al., 2011). A special type of syringe is used to harvest the plasma component after spinning. The harvested PRP is then injected back into the injured tissue (Foster et al., 2009; Raeissadat et al., 2015). The injected PRP stimulates the release of the growth factors, as previously discussed, which ultimately results in tissue healing.
Around 70% of growth factors found in PRP are released within 10 minutes, with the remaining 30% released within the first hour post injection. The lifespan of the injected PRP is around 8-10 days and during this time further growth factors can be produced and released.
How is PRP injected?
It is essential that the correct location is targeted for PRP to be effective. To achieve a safe and accurate procedure, PRP injections should be ultrasound guided. At Complete all our injections are ultrasound guided. During an ultrasound guided injection, the injured tissue is identified and targeted. The progression of the needle can be monitored throughout the procedure in real-time, ensuring a safe and accurate injection.
Is PRP a onetime only injection or do I need multiple injections?
Many patients feel the benefit from a single injection. However, it has been stated that due to the complexity and duration of the healing process a single dose of PRP has limited ability to improve tissue health (Foster et al., 2009). Common consensus in the research recommends that PRP treatment be completed as a series of three injections one month apart for the maximum potential benefits to be achieved (Gormeli et al., 2015).
PRP injections are a safe and effective way to aid the healing process, but it is essential that the underlying cause of your pain be addressed. A course of physiotherapy is highly recommended after PRP treatment. Ensuring you are as strong and flexible as possible will give you the best chance of avoiding a recurrence of your symptoms.
What can PRP successfully treat?
There is an ever-growing body of research surrounding PRP and musculoskeletal pathology. Below is a brief synopsis of what pathologies can be successfully treated using PRP. As new research is being published the list of conditions which could benefit from PRP will inevitably grow.
Knee osteoarthritis

Research has shown PRP to be an effective modality to treat osteoarthritis of the knee. Studies have shown PRP can reduce pain and increase functional ability in patients suffering with osteoarthritis of the knee and is capable of providing prolonged relief lasting up to 1 year (Bansal et al., 2021). Studies suggest that patients suffering from mild to moderate degenerative changes respond most favourably to PRP injections when compared to patients with more significant knee pathology (Gormeli et al., 2015; Raeissadat et al., 2015).
A systematic review postulated that introducing PRP into a joint could do more than just treat the degenerative changes of the meniscus (a precursor to osteoarthritis) but that it may have a wider effect on the internal environment of the joint which in itself may produce positive clinical outcomes (Filardo et al.,2013). For more information, please follow this osteoarthritis of the knee link.
PRP and tendons
Tendons are strong tensile structures which connect a muscle to the bone. They transmit forces generated by the muscle to the skeleton, creating movement of the underlying joint. Tendons are a common site for pathology to occur. A tendon which has become irritated and inflamed is known as tendonitis. When a tendon is subjected to multiple episodes of tendinitis the healing process can become impaired resulting in the formation of scar tissue which in turn produces a chronically weakened tendon. This is known as tendinosis. PRP has been shown to have positive effects for tendinopathic tendons (Pauloni et al., 2011; Zhou et al., 2015).
Two types of cells can be found specifically in tendon tissue – tenocyte cells and tendon stem cells. Tendon stem cells play a significant role in tendon tissue repair. PRP has been shown to stimulate these key cells resulting in tendon healing (Zhou et al., 2015).
Research supports the use of PRP for treating many tendon conditions including:
Tennis elbow pain
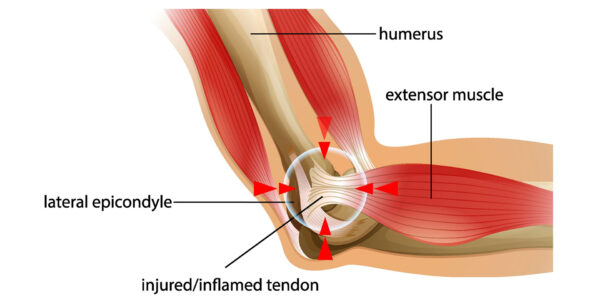
Research has revealed PRP to be capable of reducing the pain associated with tennis elbow as well as increase functional ability of the elbow for up to 2 years (Gosens et al., 2011). For more information about PRP in the treatment of tennis elbow please follow this link.
Rotator cuff tendon pain
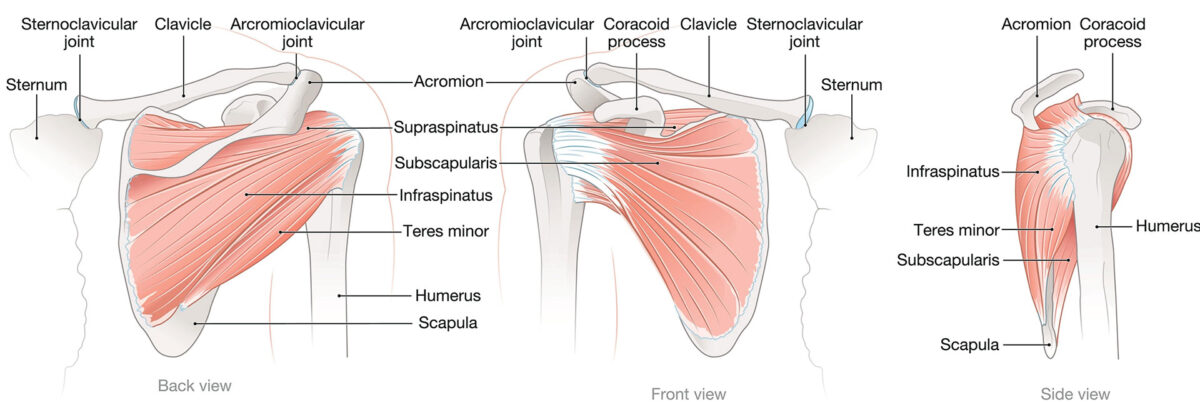
A recent systematic review supported the use of PRP injections for rotator cuff pathology (Shariff et al., 2021). This review stated that PRP was significantly more effective at controlling medium to long term pain (up to 24 weeks) when compared to other treatment options including rehabilitation exercises. This review also reported PRP to be safe and effective for shoulder rotator cuff pain, although a short term (3 days) transient increase in pain may be experienced (Shariff et al., 2021). For more information about rotator cuff pain please follow this link.
Plantar fasciitis

A high-quality systematic review conducted by Hurley et al. (2020) reported that PRP can provide superior long term (6-12 months post injection) improvements in pain and function for patients suffering from plantar fasciitis when compared with corticosteroids. There was no difference in outcomes between corticosteroids and PRP in the short to midterm. For more information about plantar fasciitis please follow this link.
During an appointment at Complete one of our expert clinicians will assess you using both clinical tests and a diagnostic ultrasound scan. All our clinicians that perform PRP injections are fully trained physiotherapists, musculoskeletal sonographers and phlebotomists, so once your diagnosis has been confirmed, and PRP is considered appropriate, an ultrasound guided PRP injection can be completed in the same session.
For further information regarding PRP or if you have any questions, please contact us on 0207 482 3875 or email injections@complete-physio.co.uk.


